ISOLATION, IDENTIFICATION AND ANTIMICROBIAL SUSCEPTIBILITY OF UROPATHOGENIC ESCHERICHIA COLI AND KLEBSIELLA SPP
Глинская Е.В.1, Аль-Баяти Б.М.2, Нечаева О.В.3, Лунева И.О.4
1Кандидат биологических наук, Саратовский государственный университет (Россия), 2Кандидат биологических наук, Багдадский государственный университет (Ирак), 3,4Кандидат биологических наук, Саратовский государственный медицинский университет (Россия)
ВЫДЕЛЕНИЕ, ИДЕНТИФИКАЦИЯ И ЧУВСТВИТЕЛЬНОСТЬ К АНТИБИОТИКАМ УРОПАТОГЕННЫХ ШТАММОВ ESCHERICHIA COLI AND KLEBSIELLA SPP
Аннотация
Проведено исследование возбудителей уропатогенных штаммов и их чувствительности к антибиотикам. Культивирование и идентификацию микроорганизмов проводили с помощью стандартных методов. Чувствительность бактерий к антибиотикам осуществляли методом диффузии в агар. Результаты показали, что в 69,5% образцов возбудителями являлись бактерии E. coli и Klebsiella spp. (55,5% - E. coli, 14% - Klebsiella spp.). Все изоляты E. coli и Klebsiella spp. были чувствительны к имипенему и амикацину, 87% штаммов - к нитрофурантоину. Высокий уровень устойчивости изолятов наблюдался к ампициллину (97%), аугментину (89%), триметоприм-сульфаметоксазолу (83,5%), налидиксовой кислоте (79%), пиперациллину (78%), цефотаксиму (70,5%), и гентамицину (65,5%).
Ключевые слова: инфекции мочевыводящих путей, Escherichia coli, Klebsiella spp., чувствительность к антибиотикам.
Glinskaya E.V.1, Al-Bayati B.M.2, Nechaeva O.V.3, Luneva I.O.4
1PhD in Biology, Saratov State University (Russia), 2 PhD in Biology, University of Baghdad (Iraq), 3,4PhD in Biology, Saratov State Medical University (Russia)
ISOLATION, IDENTIFICATION AND ANTIMICROBIAL SUSCEPTIBILITY OF UROPATHOGENIC ESCHERICHIA COLI AND KLEBSIELLA SPP
Abstract
The current study was done to demonstrate the distribution and antimicrobial susceptibility patterns of Escherichia coli and Klebsiella spp. isolated from patients with urinary tract infection (UTI) in the community. Specimens were cultured, examined, and identified by standard methods (API 20E). The antimicrobial susceptibility test was done by disc diffusion technique. Our results demonstrated that 69.5% specimen showed positive cultures for E. coli and Klebsiella spp.; 55.5% for E. coli and 14% for Klebsiella spp., 30.5% samples showed positive culture for other bacterial uropathogens. Regarding the antimicrobial susceptibility patterns, all the isolates of E. coli and Klebsiella spp. were sensitive to imipenem and amikacin (100%), whereas (87%) of them were sensitive to nitrofurantion. However, high levels of resistance were seen against ampicillin (97%), augmentin (89%), trimethoprim-sulfamethoxazole (83.5%), nalidixic acid (79%), piperacillin (78%), cefotaxime (70.5%), and gentamycin (65.5%).
Keywords: Urinary tract infection, Escherichia coli, Klebsiella spp., Antibiotic susceptibility.
Urinary tract infections (UTIs) are one of the most frequently encountered infections in both inpatient and outpatient settings [1]. Women are more prone to have UTIs than men, with a higher incidence in older people, pregnants, and diabetes [2]. Many substances (soap, bubbles bath, stool, or clothing) can cause soreness of urethra (most predominant site of infection), make it easier for bacteria to invade and multiply [3, 4]. Most of UTIs are caused by gram negative bacteria, generally Enterobacteriaceae, and mainly by E. coli and Klebsiella spp. [5, 6].
Uncomplicated UTIs are treated with antibiotics [2]. The increased utilization of antibiotics has contributed to greater resistance among urinary pathogenic bacteria to many antibiotics that are typically used in the treatment of UTIs [7]. Therefore, the current study aimed to identify the relation of E. coli and Klebsiella spp. with UTIs and their antimicrobial susceptibility patterns.
A total of 325 urine specimens were collected from patients aged 6-76 years with clinical symptoms suspected to be UTI. Specimens (midstream urine) were cultured on MacConkey’s agar, and the isolated colonies were identified by standard methods and API 20E [8]. Antimicrobial susceptibility test was performed by disc diffusion method using Muller-Hinton agar. The following antibiotic discs were used: Amikacin (A; 30 μg), Ampicillin (AMP; 10 μg), Augmentin (amoxicillin-clavulanic acid) (AMC; 30 μg), Cefotaxime (CTX; 30 μg), Gentamicin (GM; 10 μg), Imipenem (IPM; 10 μg), Nalidixic acid (NA; 30 μg), Nitrofurantion (F; 300 μg), Piperacillin (PIP; 100 μg), and Trimethoprim-sulfamethoxazole (SXT; 23.75 μg).
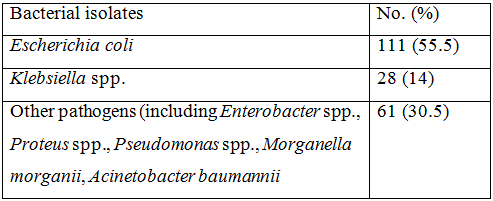
The current study demonstrates the distribution and antimicrobial susceptibility patterns of E. coli and Klebsiella spp. in UTI. Our results revealed that 200 (61.5%) specimens gave positive urine cultures for uropathogens, 100 (31%) gave negative urine cultures, and 25 (8%) exhibited mixed microbial growth. The appearance of negative urine cultures were also documented in other studies [9, 10]. This may be related to the presence of other pathogens (fungi, viruses, or slow growing organisms), or organisms that cannot be grow on ordinary culture media. Regarding the etiological agents, E. coli and Klebsiella spp. were the highest between the uropathogens, 111 (55.5%) and 28 (14%), respectively. Such rates were also seen in other studies [9, 10], mentioned an isolation rate ranged (40-70%). The results are shown in table (1).
Table 1 - Distribution of urinary pathogens (N = 200).
Our results demonstrated that 51 (37%) of males and 88 (63%) of females show positive presence of E. coli and Klebsiella spp. in their urine specimens, and this was compatible with other studies worldwide [11 - 13].
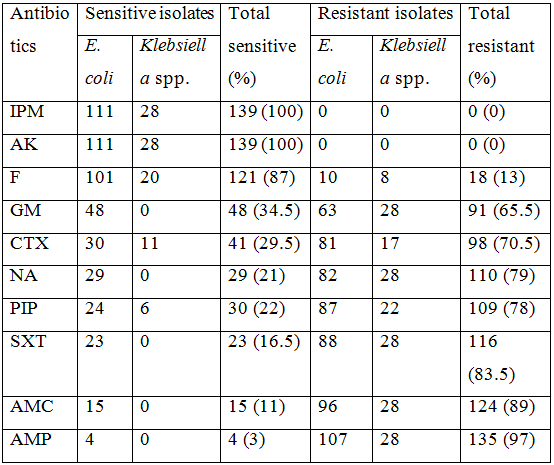
The antimicrobial susceptibility patterns of the isolates were shown in table (2). The isolates exhibited a wide difference in their susceptibility toward the tested antibiotics. All E. coli and Klebsiella spp. isolates were sensitive to imipenem and amikacin (100%), while (87%) of the isolates were sensitive to nitrofurantoin. Low rates of sensitivity were also noticed toward other tested antibiotics. Our results were in agreement with other studies worldwide [9, 10, 13]. However, (97%) of the isolates were resistant to ampicillin, (89%) to augmentin, (83.5%) to trimethoprim-sulfamethoxazole, (79%) to nalidixic acid, (78%) to piperacillin, (70.5%) to cefotaxime, and (65.5%) to gentamycin. Low rates of resistance were noticed with the other used antibiotics. Such resistance rates were also reported in other countries [14, 15]. This may be due to the excessive use of such antibiotics at primary health care level, or to the production of TEM β-lactamases. TEM-1 is the most commonly encountered β-lactamase in gram negative bacteria, and up to (90%) of the resistance is due to its production [16].
Table 2 - Antimicrobial susceptibility profile of the isolates (N = 139).
Based on the findings of this study, it is concluded that UTI affected females more than males. The main organisms causing UTIs are E. coli and Klebsiella spp. Almost all isolates show resistant patterns to the commonly prescribed antibiotics. Therefore, in blind therapy of suspected UTIs, imipenem, amikacin, and nitrofurantion were the drugs of choice.
References
- Arslan, H; Azap, O.K.; Onder, E.; and Timurkaynak, F. Risk factor for ciprofloxacin resistance among E. coli strains isolates from community acquired UTI in Turkey. J. Antimicrobial Chemotherapy. 2005; 56: P. 914-918.
- Schaeffer, A.J.; Foxman, B.; and Tracy, E. Urinary tract infections in adults, J: National Kidney and Urological Diseases information clearing house publication No. 07-4807. 2007.
- Conway, P.H.; Canaan, A.; Zaoutis, T.; Henry, B.V.; Grundmeier, R.W.; and Keren, R. Recurrent urinary tract infection in children, risk factor and association with prophylactic antimicrobials. J. American Medical Association. 2007, 11: 298 (2): P. 179-186.
- Karbwsky, J.A.; Jones, M.E.; Thornsberry, C.; Friedland, I.R.; and Sahm, D.F. Trends in antimicrobial susceptibilities among enterobacteriaceae isolated from hospitalized patients in the United States from 1998 to 2001. J. Antimicrobial Agents and Chemotherapy. 2003. 47: P. 1672-1680.
- Yamamoto, S. Molecular epidemiology of uropathogenic E. coli. J. Infection and Chemotherapy. 2007; 13: P. 68-73.
- Lorenzo-Gómez, M.F.; Padilla-Fernández, B.; García-Criado, F.J.; Mirón-Canelo, J.A.; Gil-Vicente, A.; Nieto-Huertos, A.; and Silva-Abuin, J.M. Evaluation of a therapeutic vaccine for the prevention of recurrent urinary tract infections versus prophylactic treatment with antibiotics. International Urogynecology J. 2013, 24: P.127-134
- Salvatore, D.J. and Resman-Targoff, B.H. Treatment Options for Urinary Tract Infections Caused by Extended-Spectrum Β-Lactamase-Producing Escherichia coli and Klebsiella pneumonia. J. Academic Hospital Medicine. 2015, Vol. 7, Issue 1.
- Health Protection Agency. Investigation of Urine. UK Standards for Microbiology Investigations. 2012. B 41, Issue 7.1: P.1-41. Available from http://www.hpa.org.uk/SMI/pdf.
- Kareem, I.J. and Raheed, I.Y. Antibiotic Susceptibilities of Gram Negative Aerobic Bacteria Isolated from Urinary Tract Infections in Community. Iraqi J. Medical Sciences. 2011, 9 (4): P. 295-300.
- Mahmood, M.A. Prevalence and Antimicrobial Susceptibility of Pathogens in Urinary Tract Infections. J. Al-Nahrain University. 2011, 14 (4): P. 146-152.
- Adedeji, B.A. and Abdulkadir, O.A. Etiology and antimicrobial resistance pattern of bacterial agents of urinary tract infections in students of Tertiary Institusions in Yola Metropolis. Advances in Biological Research. 2009, 3 (3 – 4): P. 67-70.
- Mehr, M.T.; Khan, H.; Khan, T.M.; Iman, N.U.; Iqbal, S.; and Adnan, S. E. coli urine super bug and its antibiotic sensitivity: A prspective study. International J. Medical Sciences. 2010, 18 (2): P. 110-113.
- Kebira, A.N.; Ochola, P.; and Khamadi, S.A. Isolation and antimicrobial susceptibility testing of Escherichia coli causing urinary tract infections. J. Applied Biosciences. 2009, 22: P. 1320-1325.
- Ahmed, A.A.; Osman, H.; Mansour, A.M.; Musa, H.A.; Ahmed, A.B.; Karrar, Z.; and Hassan, H.S. Antimicrobial agent resistance in bacterial isolates from patients with diarrhea and urinary tract infection in Sudan; American J. Tropical Medicine and Hygiene. 2000, 63, P. 259-263.
- Ndugulile, F.; Jureen, R.; Harthug, S.; Urassa, W.; and Langeland, N. Extended spectrum β-lactamases among Gram-negative bacteria of nosocomial origin from an intensive care unit of a tertiary health facility in Tanzania. BMC Infectious Diseases. 2005, 5 (86).
- Bradford, P.A. Extended-spectrum β-lactamases in the 21st century: Characterization, epidemiology, and detection of this important resistance threat. Clinical Microbiology Reviews. 2001, 14: P. 933-951.