КЛИНИКО-ЭЛЕКТРОФИЗИОЛОГИЧЕСКИЕ ОСОБЕННОСТИ ПОСТТРАВМАТИЧЕСКИХ НЕВРОПАТИЙ
Чичановская Л.В. 1, Соловьева А.В. 2, Назаров М.В. 3
1 доктор медицинских наук, заведующая кафедрой неврологии, медицинской генетики и нейрохирургии, 2 доктор медицинских наук, заведующая кафедрой поликлинической терапии и основ доказательной медицины, 3 аспирант кафедры неврологии, медицинской генетики и нейрохирургии, Тверской Государственный Медицинский Институт
КЛИНИКО-ЭЛЕКТРОФИЗИОЛОГИЧЕСКИЕ ОСОБЕННОСТИ ПОСТТРАВМАТИЧЕСКИХ НЕВРОПАТИЙ
Аннотация
Поражение периферических нервов по данным ВОЗ составляют от 8 до 10% от общей заболеваемости и до 50% всех заболеваний нервной системы. Проблема заболеваний периферической нервной системы является одной из ведущих в неврологии. В неврологических стационарах количество больных с этими заболеваниями достигает 65-70%. Заболевание широко распространено среди лиц трудоспособного возраста. Так 76% случаев с временной утратой трудоспособности составляют заболевания периферической нервной системы (ПНС), что подтверждает социальную значимость данной.
Ключевые слова: посттравматическая невропатия, компрессионно-ишемическая невропатия, электронейромиография.
Chichanovskaya L.V. 1, Soloveva A.V. 2, Nazarov M.V. 3
1 MD, 2 MD, 3 postgraduate student, Tver State Medical University
CLINICAL AND ELECTROPHYSIOLOGICAL FEATURES OF POST-TRAUMATIC NEUROPATHIES
Abstract
According to the WHO, peripheral nerve injuries make up to 8-10% of the total morbidity and up to 50% of the disorders of the nervous system. The problem of peripheral nervous system disorders is one of the most important in today’s neurology. Patients with these disorders comprise 65-70% of all patients in neurological departments of hospitals. The prevalence is high among working population. Disorders of the peripheral nervous system account for 76% of all cases of temporary disability, which proves social significance of the problem.
Keywords: post-traumatic neuropathy, compressive-ischemic neuropathy, electroneuromyography.
Introduction. Damage to the nerve trunks of extremities occurs due to man-caused and natural disasters, gun shot, road, sport, industrial, off-the-job injuries. The number of iatrogenic injuries is also increasing: nerve compression due to incorrect application of tourniquets, plaster casts, rough manipulations during repositioning of bone fragments or reducing relocation, during osteosynthesis, etc. Prevalence of peripheral nerve injuries, long inpatient treatment, and frequent disability determine medical and social significance of the problem of traumatic neuropathies.
The aim of the research was to study the dependence of clinical and electrophysiological features of post-traumatic neuropathies on the etiological and temporal factors.
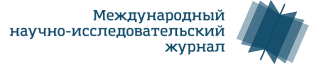
Material and methods. We evaluated a series of 28 patients with acute post-traumatic neuropathy 2 weeks after injury and 4 weeks after injury. The patients were divided into 2 groups depending on the underlying cause. Group 1 included 18 patients with compressive-ischemic neuropathies (64.3%), Group 2 included 10 patients (35.7%) with post-traumatic neuropathies caused by stab wounds.
For objective assessment of the neurological deficit severity in patients with post-traumatic neuropathies, we used the classification offered by S.N. Zhulev (1996):
1st degree (mild) – presence of paresthesias, pain syndrome, mild vegetative disorders in the area innervated by the affected nerve;
2nd degree (moderate) – presence of pareses and hypotrophy of the muscles innervated by the affected nerve, moderate vegetative disorders and paresthesias in the area innervated by the affected nerve, pain syndrome;
3rd degree (severe) – presence of pareses and hypotrophy of the muscles innervated by the affected nerve, severe vegetative disorders and paresthesias in the area innervated by the affected nerve, pain syndrome.
The patients in both groups underwent stimulation electroneuromyography to assess the excitation conduction velocity (ECV) along the motor and sensory fibers, M-response and sensory response amplitudes. 4 weeks after injury the patients had a second clinical and electrophysiological examination.
Results and discussions. We carried on a clinical and electrophysiological investigation of the patients during the acute period (up to 2 weeks). The following results were received.
Fig 1. Prevalence of post-traumatic neuropathies depending on the cause.
As we can see in Fig. 1, depending on the cause, the subjects were divided into 2 groups. Group 1 included 18 patients with compressive-ischemic neuropathies (64.3%), Group 2 included 10 patients (35.7%) with post-traumatic neuropathies caused by stab wounds.
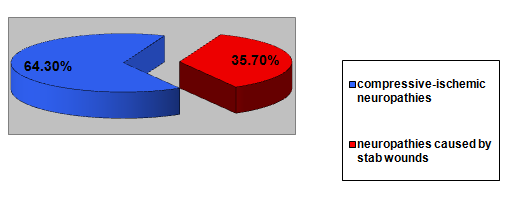
In addition, the subjects were divided according to the severity of neurological deficit.
Fig. 2. Prevalence of post-traumatic neuropathies depending on the severity of neurological deficit.
Severe neurological deficit was diagnosed in 5 patients (27.8%) in Group 1 and in 6 patients (60%) in Group 2; moderate neurological deficit was diagnosed in 10 patients (55.55%) in Group 1 and in 3 patients (30%) in Group 2; mild neurological deficit was diagnosed in 3 patients (16.65%) in Group 1 and in 1 patient (10%) in Group 2. As seen in Fig. 2, there is sufficient prevalence of severe neurological deficit in patients with neuropathies caused by stab wounds (Group 2). In Group 1 (compressive-ischemic neuropathies), moderate neurological deficit is prevalent.
Unlike patients with compressive-ischemic neuropathies, patients with neuropathies caused by stab wounds had more severe clinical manifestations associated with the direct damage to the nerve by a sharp object, which resulted in axonal nerve damage.
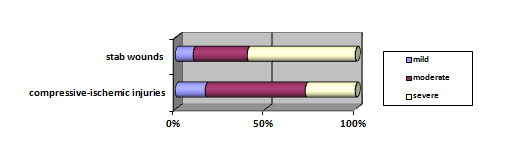
Another aim of our study was to assess the electroneuromyographic parameters (ECV along the motor and sensory fibers, M-response and sensory response amplitudes).
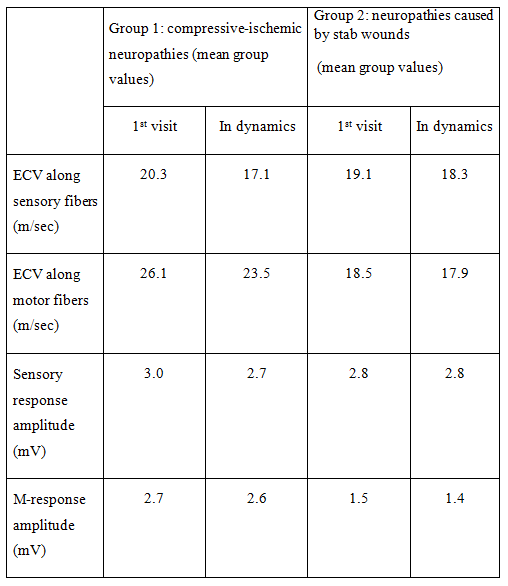
Table 1. Electroneuromyographic parameters in patients with post-traumatic neuropathies (2 weeks after injury)
Analyzing the electroneuromyographic parameters in patients with compressive-ischemic neuropathy, we revealed decrease in ECV along the sensory fibers – 20.3 m/sec (normally – over 50 m/sec). Depending on the severity of the nerve damage, the decrease in ECV varied, being 38.5 m/sec for the mild damage, 28.2 m/sec for moderate damage, 15.2 m/sec for severe damage. The mean value of the decrease in the amplitude of the sensory response resulting from compression was 3.0 mV (normally – over 8.5 mV).
In patients with moderate and severe neuropathies resulting from more significant compression-induced damage, we also revealed decreased parameters of M-response. The mean ECV being 26.1 m/sec (normally – over 50 m/sec), the mean M-response amplitude was 2.7 mV (normally – over 6 mV). The parameters of M-response amplitude correlated with the severity of the damage.
The electroneuromyographic parameters in Group 2 were characterized by a more significant decrease in the M-response amplitude: the mean value was 1.5 mV (normally – over 6 mV) that also correlated with the severity of the neurological deficit. The sensory response parameters were less significant. However, there were patients with severe neurological deficit who demonstrated no sensory response with standard stimulation parameters.
The patients underwent electroneuromyography 4 weeks after injury and the data were summarized in Table 2.
Table 2. Electroneuromyographic parameters in patients with post-traumatic neuropathies in dynamics (4 weeks after injury)
As seen in Table 2, during the first 4 weeks the patients with compressive-ischemic neuropathies demonstrated decrease in the ECV along sensory fibers by 3-4 m/sec, along motor fibers by 2.5-3 m/sec. Sensory and M-response amplitudes did not change.
Patients with mild neuropathies showed decrease in ECV along sensory fibers that are more sensitive to hypoxia. Along with decrease in ECV along sensory fibers, there was a certain decrease in the sensory response amplitude, while decrease in the ECV along motor fibers was minimal.
The most significant changes in patients with mild and moderate neuropathies were decreased ECVs along sensory and motor fibers, which was a sign of demyelielation resulting from long-lasting ischemization caused by nerve compression.
In patients with stab wounds during the first 4 weeks we observed decrease in ECV along sensory and motor fibers that was a sign of demyelination probably resulting from ischemization caused by the swelling of the tissues surrounding the wound site, and trophic disorders of the nerve fiber resulting from interruption of nerve supply.
Conclusions.
- The study has shown that patients with neuropathies caused by stab wounds, unlike those with compressive-ischemic neuropathies, had more severe clinical manifestations associated with the direct damage to the nerve by a sharp object, which resulted in axonal nerve damage.
- The electroneuromyographic parameters in Group 2 were characterized by a more significant decrease in the M-response amplitude that also correlated with the severity of the neurological deficit. The sensory response values were less significant. However, we observed patients with severe neurological deficit who demonstrated no sensory response with standard stimulation parameters.
- In patients with stab wounds during the first 4 weeks we observed decrease in ECV along sensory and motor fibers that was a sign of demyelination probably resulting from ischemization caused by the swelling of the tissues surrounding the wound site, and trophic disorders of the nerve fiber resulting from interruption of nerve supply.
- Taking into consideration high incidence of the disorder and long-term temporary disability of patients with post-traumatic neuropathies, the treatment protocol of patients with extremity injuries should include consultation of a neurologist and electrophysiological methods of assessing peripheral nerves of the injured extremity to administer an adequate pathogenetic therapy based on the received data.
- The results achieved will contribute to earlier diagnostics and treatment of post-traumatic neuropathies, which will improve the recovery of the peripheral nerves after injury and shorten the disability period of patients with post-traumatic neuropathies.
References
- Julev N.M. Nevropatii. Rukovodstvo dlya vrachei. Izdatelstvo_ Sankt_Peterburgskaya medicinskaya akademiya poslediplomnogo obrazovaniya.
- Kasatkina L.F. Sanadze A.G. Klinicheskaya elektromiografiya dlya prakticheskih nevrologov. GEOTAR_Media_ 2009.
- Mumenthaler М., Schliack Н., Stohr М. Läsionen peripherer Nerven und radikulare Syndrome, 7. Auflage: Thieme, Stuttgart, 1998.
- Russell Stephen M. Examination of Peripheral Nerve Injuries: An Anatomical Approach. Thieme, 2006.