ШУМОВАЯ ЭКСПОЗИЦИЯ И ИСХОД РОДОВ: СИСТЕМАТИЧЕСКИЙ ОБЗОР СИСТЕМАТИЧЕСКИХ ОБЗОРОВ
Джамбов A.M.1, Димитрова Д.Д.2, Димитракова E.Д.3, Александрова M.A.4
1 Студент, кандидат в докторантуру, Медицинский Университет, Пловдив, 2 доктор наук по социальной медицине, доцент факультета Общественного здоровья, Медицинский Университет, Пловдив, 3 доктор наук по акушерству и гинекологии, доцент, Медицинский факультет, Медицинский Университет, Пловдив, 4 преподаватель, Медицинский колледж, Медицинский Университет, Пловдив
ШУМОВАЯ ЭКСПОЗИЦИЯ И ИСХОД РОДОВ: СИСТЕМАТИЧЕСКИЙ ОБЗОР СИСТЕМАТИЧЕСКИХ ОБЗОРОВ
Аннотация
Вступление: Учитывая распространенность шумового загрязнения в современном мире и большой процент беременных женщин, подвергнутых шумовому загрязнению, накопилось значительное число доказательств для исследования биологических механизмов и эпидемиологического риска неблагоприятных исходов родов. Результаты являются, однако, противоречивыми не только в первичных исследованиях, но и также в систематических литературных обзорах. Систематический обзор систематических обзоров (SRSRs) может стать мощным инструментом, способным решить подобного рода проблемы.
Цель: Для того, чтобы решить эту проблему, мы исследовали при проведении SRSRs отношение шумовой экспозиции на исход родов.
Материал и методы: Были иследованы руководящие принципы по проведению систематического обзора систематических обзоров, найдены базы данных с рецензируемой и малоизвестной литературой, личные архивы, был установлен контакт со специалистами в данной области. После рассмотрения четырех систематических обзоров, соответствующих критериям включения, их методологическая точность была проверена с помощью утвержденного инструмента оценки качества и была рассчитана доля дублирующих исследований.
Результаты: В соответствии с тремя средними по качеству систематическими обзорами, наши результаты доказали, что хроническое профессиональная экспозиция ≥ 80 – 85 дБ связана со значительно более высоким риском малого гестационного возраста плода / низкого веса при рождении. Единственный противоречащий систематический обзор получил самую низкую отметку.
Выводы: Профессиональное воздействие ≥ 80 - 85 дБ является фактором риска для малого гестационного возраста у плода / низкого веса при рождении. Последующие исследования должны в первую сосредоточиться на малоизученных исходах родов, качественных методах исследования и связях между психоакустическими факторами и неблагоприятными исходами родов.
Ключевые слова: систематический обзор систематических обзоров, воздействие шума, производственный шум, исход родов, беременность, малый размер плода для гестационного возраста, низкий вес при рождении.
Dzhambov A.M.1, Dimitrova D.D.2, Dimitrakova E.D.3, Alexandrova M.A.4
1 Postgraduate student, 2 PhD in Social Medicine, associate professor, 3 MD, associate professor, 4 lecturer, Medical University of Plovdiv
NOISE EXPOSURE AND BIRTH OUTCOMES: SYSTEMATIC REVIEW OF SYSTEMATIC REVIEWS
Abstract
Background: Given the prevalence of noise pollution in the Modern World and the large percentage of pregnant women exposed, considerable body of evidence has accumulated exploring the biological mechanisms and epidemiological risk for noise-attributed adverse birth outcomes. The findings are, however, discordant not only between primary studies, but in the systematic review literature as well. In such cases a systematic review of systematic reviews (SRSRs) might be a powerful tool to settle important issues such as this.
Aim: In order to address this problem we aimed at conducting SRSRs of the relationship noise exposure – birth outcomes.
Material and Methods: Established guidelines for conducting SRSRs were followed, searching databases of peer-reviewed and grey literature, personal archives and contacting experts in the field. After identifying four systematic reviews meeting inclusion criteria, their methodological rigour was checked against a validated quality assessment tool and the proportion of overlapping studies was calculated.
Results: In accordance with three moderate-to-high quality systematic reviews, our results showed convincing evidence that chronic occupational exposure to ≥ 80 – 85 dB is associated with significantly higher risk for small for gestational age/low birth weight. The only discordant systematic review received the lowest quality score.
Conclusions: Occupational exposure to ≥ 80 – 85 dB is a risk factor for risk for small for gestational age/low birth weight. Future primary studies should focus on underexplored birth outcomes, qualitative research methods and drawing links between psychoacoustic factors and adverse birth outcomes.
Keywords: systematic review of systematic reviews, noise exposure, occupational noise, birth outcomes, pregnancy, small for gestational age, low birth weight.
Introduction
Residential and occupational noise pollution has reached alarming prevalence in developed countries [1-3]. It is associated with considerable burden of disease and economic losses [4, 5]. In addition to hearing impairment [6], the non-auditory effects of noise pollution have attracted much attention in the recent decades, and while there is no longer any doubt about it being a risk factor for cardiovascular diseases [7], its effects on human reproductive outcomes are still opened to debate.
The biological mechanisms behind noise effects on birth outcomes have been studied in detail. Psychological stress has negative impact on pregnancy and fetal development [8, 9] and noise acts as a prototypal environmental stressor. Its perception is closely linked to the autonomous nervous system and hypothalamic-pituitary-adrenal axis, and through both direct and indirect pathways it results in activation of the sympathetic nervous system and release of stress hormones such as epinephrine, norepinephrine and cortisol [10-13]. The teratogenic effect of noise might be caused by placental hypoperfusion, fetal hypoxia and stimulation of maternal catecholamine release [14, 15]. Stress-release of maternal catecholamine is associated with increase in blood pressure and uterine reactivity [16]. In addition, maternal cortisol might pass through the placental barrier, thus interfering in the regulation of the fetal hypothalamic-pituitary-adrenal axis or stimulating the placenta to secrete corticotropin releasing hormone [17]; excessive production of corticosteroids might be toxic to the embryo, whereas noise intensity of about 80 dB could increase the hematoencephalic barrier’s penetrability [18]. Marked decrease in human placental lactogen in pregnant women exposed to aircraft noise has been observed as well [19].
Research on externally generated noise in human uterus suggests that attenuation by the maternal abdominal wall is low for low frequency noise and high for the high frequency range [20, 21] with an average attenuation of 11.5 dB for the frequency range 20 Hz – 20 kHz [22]. Higher exogenous noise frequencies (4 kHz) are attenuated by approximately 20 dB, whereas in the low frequency spectrum they can even be enhanced, resulting in greater intra-abdominal sound pressure [23]. Low frequency noise is common in industrial settings, and, while it might not cause annoyance, it is a putative risk factor for pregnant women [24].
In order to plan preventive interventions and take political action we need convincing evidence that noise exposure is associated with increased risk for adverse birth outcomes and pregnancy complications. Unfortunately, the results are inconclusive not only across primary studies, but in synthetic research on the topic. The study of Hohmann et al. [25] is sometimes cited as evidence of lack of effects of noise exposure on pregnancy outcomes, which does not necessarily adequately reflect the scientific reality.
Just as primary (alias original) studies have their limitations and differ methodologically, systematic reviews (SRs) are also subject to various sources of bias [26]; policy-makers and practitioners are facing a plethora of systematic reviews on a certain topic sometimes reporting conflicting results [27, 28]. For this reason in the present study we aimed at conducting a systematic review of systematic reviews (SRSRs) of the relationship noise exposure – birth outcomes. In particular, our objectives were to assess the quality of published SRs, to determine whether available data support the hypothesis about the detrimental effects of noise on birth outcomes, and to identify insufficiently covered aspects in “noise and pregnancy” literature needing further attention.
Methods
A SRSRs aims at providing summarized evidence from SRs; it identifies all published SRs on an important topic, appraises their quality and contrasts their findings [26, 29].The present study adheres to the reporting guidelines outlined by Smith et al. [26].
Sources and search strategy
A systematic search was carried out independently by two of the authors (A. D. and D. D.) and all discrepancies were resolved by consensus with a third reviewer (E. D.). Standard search protocol and data extraction sheets were developed a priori. The research question was formulated as follows: “Is there evidence of detrimental effects of chronic noise exposure (both occupational and residential) during pregnancy on fetal development, pregnancy and/or birth outcomes?” Several databases of peer-reviewed literature were scanned for papers published through October 27, 2014 using automated search engines – PubMed/MEDLINE, ScienceDirect, Web of Science, Scopus and Google Scholar. In addition, we searched the Internet using Google and Health Technology Assessments database to identify grey literature (PhD theses, official reports, conference proceedings, etc.) and PROSPERO in order to identify prospectively registered SRs. Our personal archives were searched as well. Experts in environmental medicine and obstetrics were contacted and asked to provide relevant papers from their files. Finally, key journals and reference lists of identified SRs were manually searched. All retrieved papers were hierarchically screened on three levels – titles, abstracts and full texts. Language restrictions were imposed limiting our search to English, Russian, Spanish, French and Italian. The following free-term keyword combinations were used in the respective languages: “noise + pregnancy + review”, “noise + birth outcomes + review”, “noise + reproductive outcomes + review ”.
Review selection
The following inclusion criteria were applied: reviews with clearly defined research question and conclusions, using systematic search strategy (i.e., explicit and replicable search method and inclusion and exclusion criteria) with or without complementary meta-analysis; reviews focused on occupational and/or residential noise exposure, exploring birth and/or pregnancy outcomes – low birth weight (LBW), small for gestational age (SGA), preeclampsia (PE), gestational hypertension (GH), preterm birth (PB), congenital malformations/anomalies (CM), spontaneous abortion (SA), perinatal death (PD), still birth (SB), – and including primary studies that have used objective and/or subjective assessment of noise exposure. Papers not meeting these inclusion criteria (e.g., focused solely on noise effects on children, noise exposure in intensive care units or fetal hearing development) were excluded.
Quality assessment of included reviews
Quality appraisals were made by two of the authors and any discordance was resolved by consensus with the other authors. The assessment of methodological quality of the included SRs was crucial for drawing conclusions regarding the effects of noise exposure on birth outcomes. In order to make sure that all included SRs met a minimum quality standard they were checked against AMSTAR, a validated instrument for quality assessment of SRs [30], which has been deemed suitable for SRs based on epidemiological studies [31]. AMSTAR comprises 11 items where each item scoring “yes” is awarded 1 point. The maximum quality score is 11; however, two of the items are relevant only to quantitative meta-analyses. The reasons for discordant findings were explored by following the algorithm proposed by Jadad et al. [32] after slight modification was made in accordance with the epidemiological nature of our topic. Additionally, according to Pieper et al. [33], we generated a citation matrix and calculated the proportion of overlapping primary studies for the birth outcomes in each SR, as well as the “corrected covered area” (CCA) as a measure of the degree of overlap.
Results
Overview of included studies
The literature search identified five SRs on noise exposure and birth/pregnancy outcomes [25, 34-37]. Only four of those, however, met inclusion criteria: The study of Bastos et al. [37] lacked specific focus on noise risk assessment and clear inferences; it described the methodologies of several primary studies but did not come to a conclusion regarding the noise-attributed risk for adverse birth outcomes.
Three of the four included SRs [25, 35, 36] were peer-reviewed articles, while the study of Croteau [34] was a report prepared for the Government of Quebec. All SRs focused on the relationship chronic noise exposure – birth outcomes. Hohmann et al. [25] and Croteau [34] additionally looked at noise effects on children and the risk for hearing impairment, respectively. Those outcomes, however, were outside the scope of our SRSRs and were left out of the meta-synthesis. All of the studies explored the noise-attributable risk for birth outcomes. Some of the reviews presented us with ambiguity in discerning between SGA and LBW as outcome variables [34, 35].
A priory literature search protocol was developed in all of the reviews. In most of them [25, 35, 36] at least two experts were entrusted with identification and selection of primary studies relevant to the research question. A comprehensive literature search in at least two bibliographic databases of peer-reviewed literature was carried out. As recommended [38-40], MEDLINE and EMBASE were screened in all of the reviews to ensure comprehensive coverage of the literature. Ristovska et al. [36] additionally searched Web of Science, whereas Dzhambov et al. [35] carried out a general Internet search using Google. Although the latter was an unconventional approach, due to this Google search Dzhambov et al. [35] were able to locate the report of Croteau [34] omitted by Hohmann et al. [25] and Ristovska et al. [36]. As a next step all authors considered hand-searching the reference lists of included studies. However, Hohmann et al. [25] and Croteau [34] did not search for non-peer reviewed publications and unpublished material, respectively. Ristovska et al. [36] applied no language restrictions, Hohmann et al. (25) made no mention of it, and Dzhambov et al. [35] limited their search to English, Russian and Spanish (although they used some input data from studies previously abstracted by Croteau [34]). Croteau [34] included only studies published in English and French.
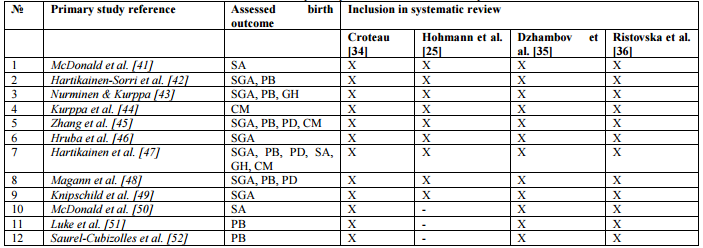
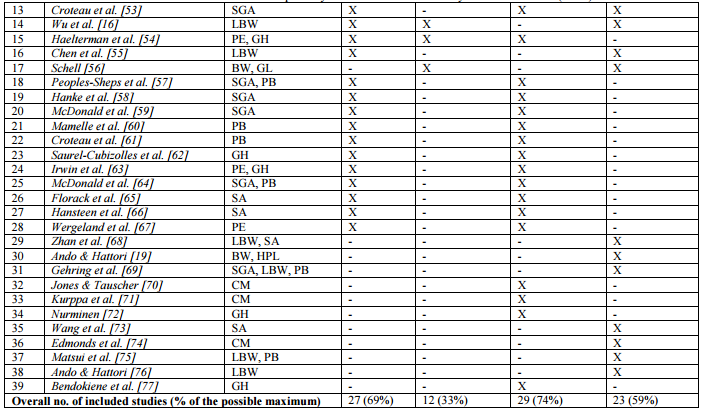
Taking a closer look at the primary studies included in each SR, we identified 9 “core” studies included in all of the reviews (See Table 1). According to the CCA values (See Table 2) the overlap of primary studies was very high (> 15%) with respect to all birth outcomes [33].
Table 1. Citation matrix of primary studies included in the systematic reviews
Note. SGA – small for gestational age, LBW – low birth weight, BW – birth weight, SA – spontaneous abortion, PB – preterm birth, PD – perinatal death, PE – preeclampsia, GH – gestational hypertension, CM – congenital malformations, HPL – human placental lactogen, GL – gestational length
Moreover, none of the reviews was able to cover all eligible studies (n = 39) on noise and birth outcomes. Some of the authors [35, 36] stated that due to technological restrictions they had limited access to some of the full texts. This might be expected, given that most of the articles were published several decades ago, which made it difficult to find the full texts online or contact the authors. In addition, Dzhambov et al. [35] lacked sufficient funding and institutional subscription to some journals, which was a major hindrance to obtaining important articles. The authors partially compensated for this by using already abstracted by previous reviews data about those articles; they also extracted some effect size estimates from the report of Croteau [34].
Table 2. Overlapping studies included in systematic reviews (corrected covered area)
Note. SGA – small for gestational age, LBW – low birth weight, SA – spontaneous abortion, PB – preterm birth, PD – perinatal death, PE – preeclampsia, GH – gestational hypertension, CM – congenital malformations
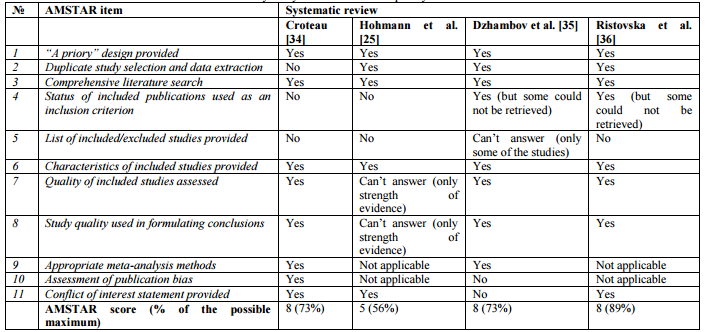
Quality appraisal
The quality of SRs was checked against AMSTAR (See Table 3). All reviews applied some kind of protocol to assess the methodological quality of individual studies. Hohmann et al. [25] formulated their conclusions based on the level of evidence of the included primary studies and followed the Scottish Intercollegiate Guidelines Network in order to rate the studies based on their design (i.e., cohort, cross-sectional, case-control, etc.). The other three review teams developed quality protocols specific to the research question. Croteau [34] implemented a complex and sophisticated scoring system; biological plausibility and different sources of bias were quantified and these quality scores were then used in meta-regressions in order to obtain adjusted pooled estimates. Dzhambov et al. [35] partially adopted the scoring system of Croteau [34] and, because they conducted quality effects meta-analyses, they were able to utilize the quality scores in the statistical analyses to re-distribute inverse variance weights away from lesser quality studies. The quality criteria of Ristovska et al. [36] draw on the Newcastle–Ottawa quality assessment scale for case-control and cohort studies [78], which, although less detailed than Croteau’s [34] checklist, addressed the key features of each study – study design, assessment of noise exposure and birth outcomes, adjustment for relevant confounders and other sources of bias.
Table 3. Summary of systematic reviews quality assessed with AMSTAR
Two of the reviews were followed by a meta-analysis [34, 35]. While Hohmann et al. [25] argued that due to methodological heterogeneity a quantitative meta-analysis was not feasible, several years earlier Croteau [34] reported quantitative results based on DerSimonian-Liard random effects meta-analyses and meta-regressions, and recently Dzhambov et al. [35] reanalyzed and updated their results applying a new method known as the quality effects model. The quality effects model is considered superior to the random effects model as it allows incorporating study quality scores in the statistical procedures for calculating pooled estimates [79].
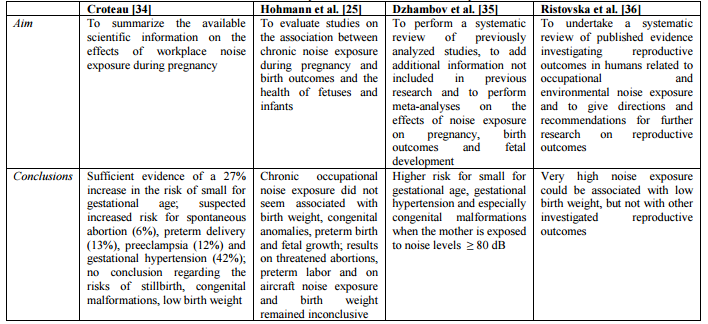
Main studies’ findings
SGA/LBW was the only outcome about which three out of the four reviews [35-36] agreed that noise exposure of over 80-85 dB during pregnancy increased the risk for (See Table 4). The two meta-analyses reported an OR of 27% based on meta-regression-adjusted results [34] and a RR of 19% based on the quality effects model [35]. The qualitative meta-synthesis of Ristovska et al. [36] supported the association between noise exposure and LBW.
Table 4. Aim and conclusions of systematic reviews on noise exposure and birth outcomes
With respect to other birth outcomes, only some of the reviews found negative effects of noise, and therefore the evidence is still inconclusive. Croteau [34] reported suspected OR of 6% for SA, 13% for PB, 12% for PE and 42% for GH if the woman has been exposed to > 85 dB during her pregnancy. The more conservative approach of Dzhambov et al. [35] yielded pooled RR of 33% for SA, 5% for PB, 7% for PE, 27% for GH, 27% for PD and 47% for CM, when comparing noise exposure of < 80 dB vs. > 80 dB. Noteworthy, the only outcomes in the review of Dzhambov et al. [35] for which the pooled risk estimates reached statistical significance (95% CI did not overlap zero) were SGA, GH and CM.
Discussion
Synopsis of principal findings
We conducted SRSRs of the relationship noise exposure – birth outcomes. Four SRs were identified. Two of them were followed by a meta-analysis. We found that there is convincing evidence that chronic occupational exposure to ≥ 80 – 85 dB is associated with significantly higher risk for SGA/LBW. These inferences are in line with the conclusions of three moderate-to-high quality reviews. The only SR which did not find sufficient evidence to support this hypothesis [25], noteworthy, received the lowest quality score on AMSTAR; likewise, the limitations of their literature search were more pronounced in comparison to those of the other studies.
It is disputable whether in meta-analyses of epidemiological studies we should be adhering strictly to statistical significance, or rather be interested in the direction and magnitude of the pooled effect. For the sake of being conservative and not overestimate the effect, we suggest a risk for SGA of about 19% (95% CI: 1.03, 1.38) for mothers exposed to > 80 – 85 dB during pregnancy. We are willing to give priority to the findings of Dzhambov et al. [35] because we believe their statistical approach is better justified by the primary research heterogeneity. Moreover, for some of the studies they calculated RR or converted OR to RR, which yielded more conservative estimates. These are best-guess results that we currently have, but the risk is probably somewhat lower given that not all input effects sizes in Dzhambov et al.’s [35] analyses were RRs. A more robust quality scoring protocol giving larger penalty for some quality elements such as adjustments for relevant confounders would generate more accurate study weights.
Quality of the reviews
The review of Ristovska et al. [36] received the highest score on AMSTAR. The two meta-analyses [34, 35] scored somewhat lower, and the review of Hohmann et al. [25], the only one rejecting the hypothesis of negative effects on birth outcomes, was of lower quality. The common limitation of the reviews was the lack of detailed list of both included and excluded studies. On the other hand, the fact that specific checklists were developed for the purpose of assessing methodological quality of included studies is commendable. However, Hohmann et al. [25] confined to evaluating the level of evidence associated with each primary study’s design. The latter, along with the limited literature search of the authors, are the causes for the lower AMSTAR score of Hohmann et al. [25]
Strengths and limitations
SRSRs have gained prominence over the last years and their numbers are rising [29], as they offer advantages over SRs of primary studies [33]. Although a SRSRs does not generate new information that was not available before, is a powerful tool for addressing urgent topics especially if there is controversy or a number of published SRs of various quality and discordant findings. By highlighting and identifying reasons for this discordance, it presents a higher level of data synthesis which can be used to reconcile disparate findings.
This is the first SRSRs on noise exposure and birth outcomes. Nieuwenhuijsen et al. [80] published a summary of meta-analyses of environmental exposures and pregnancy outcomes and described their methodologies. Not surprisingly, the effects of noise were not tackled due to the limited synthetic research at that time. Thus, our paper fills this gap in the literature and gives an answer as to the risk for noise-related SGA/LBW.
Experts have found that addressing the discordance of included reviews is uncommon in SRSRs; the same refers to the assessment of their quality [29]. On the contrary, our SRSRs followed the guidelines proposed by Smith et al. [26] and assessed the methodological quality of each included review using a validated quality checklist, the AMSTAR tool. AMSTAR is one of the most frequently used quality assessment instruments in this kind of synthetic research [29]. Discordance in the reviews was critically discussed and the proportion of overlapping studies was quantified and taken into consideration.
However, there are few limitations of the included SRs that need to be addressed. First, it is noteworthy that the meta-analysis of Croteau [34] was missed by the searches of not only Nieuwenhuijsen et al. [80], but Hohmann et al. [25] and Ristovska et al. [36] as well. If it were not for the efforts of Dzhambov et al. [35] to trace it down, the study of Croteau [34] would still be widely unknown. The fact that it is written in French, along with the fact that it was accessed through Google, rather than a scientific search engine, might explain why there was no previous mention of it in the relevant literature. Conversely, because Dzhambov et al. [35] adopted the quality scoring protocol of Croteau [34] in order to ensure compatibility between the two studies, it is very difficult to interpret those two reviews independently from each other. It is to be expected that any technical or methodological flaws in Croteau [34] would automatically be inherited in the analyses of Dzhambov et al. [35], especially since some of the effect sizes reported by Croteau [34] were used by Dzhambov et al. [35] directly without scrutiny or any means of checking their accuracy. Furthermore, neither Croteau [34], nor Dzhambov et al. [35] seemed to discriminate between LBW and SGA, although the former is defined as birth weight < 2500g regardless of the gestational age, and the latter takes gestational age into account. The authors relied on the fact that the two terms can often be applied interchangeably.
Another important difference between the reviews is that some of them focused only on occupational noise exposure [34], whereas the rest also included studies dealing with residential exposure. While this is a possible source of exposure misclassification bias, the conclusions regarding the risk for SGA/LBW are based exclusively on occupational exposure studies.
Critics might also argue that, in order for SRSRs to be feasible, none or very few duplicate studies in the included reviews should be identified. We observed very high proportion of overlapping studies, although only nine were covered by all SRs. This introduces possible bias. Likewise, due to the fact that only two meta-analyses were found, and because they included the same primary studies, we did not conduct a meta-analysis of meta-analyses which would have given too much statistical power to multiple included primary studies [26]. Nevertheless, the overlap does not preclude synthetizing these SRs because they had adopted different methodologies. The conclusion regarding the risk for SGA/LBW provides additional evidence for the detrimental effects of noise exposure, since the results of these SRs are the same regardless of their methodology; on the other hand, we investigated the reasons for the discordance originating from Hohmann et al. [25].
Although currently there is no general rule of thumb to suggest what the minimum number of SRs to be included in SRSRs is, after contacting an expert in SRSRs methodology, we concluded that four SRs should be sufficient to add value to the research question and reinforce the need for alternative approaches in conducting primary studies. This notion is heuristically supported by previous SRSRs [81]. Moreover, even empty systematic reviews are possible when they focus on highly specific questions or when stringent minimum quality criteria for inclusion in the review have been imposed [82].
Since SRs are liable to publication bias within the primary research data, any such bias may have been inherited in our study. Primary studies were not obtained or reviewed and their quality was not assessed. Rather, we determined the appropriateness of the methods used in each SR to assess this quality and to incorporate it in the review [32]. Whether additional searches for primary studies should be carried out at the time of conducting SRSRs still has not received definitive answer [29]. The same refers to any attempt to replicate the search strategy or data synthesis of the reviews. We relied on the peer-review procedure that most review had undergone. Also, the scientific reputation of the venues where the reviews were published was not scrutinized, and only the reported methodology in each of them was taken into consideration when establishing their overall credibility [26]. Furthermore, the AMSTAR tool measures “the quality of the conduct of a review and therefore cannot guarantee that the results or conclusions of a review are in line with the underlying evidence” [29].
Considerations for future research
All included reviews were published in the past five years. However, it might be prudent to routinely screen relevant databases and monitor the research activity in the field in order to update the SRs on the topic as well as this SRSRs. Our study reinforces the need for a focus on birth outcomes other than SGA/LBW for which currently there is no need for additional SRs. Except for SGA/LBW and possibly GH, all other birth outcomes are either not sufficiently covered by published primary research, or the results are largely contradictory. Likewise, data regarding residential noise exposure and its effects on human pregnancy are unsufficient. Aircraft noise, in particular, should be studied since it often reaches high levels perceived as more annoying than corresponding noise from other traffic sources.
Additional knowledge might be gained through alternative methodological approaches as well. Applying qualitative research methods (e.g., cognitive interviews, phenomenological/phenomenographical approaches, introspective techniques, etc.) might help discover the psychosocial mechanisms underlying the effects of noise as an environmental stressor. As we know, some of the effects of noise exposure depend on how it is being perceived, what activities are disturbed, what our attitude and individual sensitivity are, etc. Conversely, personal resources, emotional equilibrium, attitudes and beliefs have also been linked to birth outcomes [83]. Screening programs for psychosocial risk factors associated with fetal development are warranted, since biomedical factors account for about 50% of some adverse birth outcomes [84]. Therefore, by understanding these psychoacoustic premises we might implement behavioral and psychological preventive measures which might be particularly viable for pregnant women exposed to high noise at work. Along with noise control engineering solutions, protective equipment and legislation, which ultimately reduce noise exposure, a more person-centered prophylaxis might reduce the susceptibility to noise stress.
Finally, we recommend adjustments for individual noise sensitivity in future studies. In accordance with Hohmann et al. [25], we hypothesize that by relating noise sensitivity and the perceived acoustic environment to birth outcomes, we will hopefully not only improve the explanatory power of our statistical models, but we will identify key links that can be targeted and modified.
Conclusions
In accordance with three moderate-to-high quality systematic reviews, our results showed convincing evidence that chronic occupational exposure to ≥ 80 – 85 dB is associated with significantly higher risk for small for gestational age/low birth weight. Future primary studies should focus on underexplored birth outcomes, qualitative research methods and drawing links between psychoacoustic factors and adverse birth outcomes.
Conflict of interest statement
This study did not receive external funding and the authors received no financial incentives. One of the included reviews is authored by members of the present study authors’ team, therefore possible bias cannot be ruled out, although best efforts were made to conduct objective quality assessment.
References
- European Commission. Green paper on future noise policy // Brussels. -1996 [displayed 20 October, 2014]. Available at http://ec.europa.eu/environment/noise/greenpap.htm.
- World Health Organization (WHO). Occupational noise: Assessing the burden of disease from work-related hearing impairment at national and local levels // Environmental Burden of Disease Series, No. 9. WHO Document Production Services, Geneva, Switzerland. - [displayed 20 October, 2014] Available at http://www.who.int/quantifying_ehimpacts/publications/en/ebd9.pdf.
- Goines L., Hagler L. Noise pollution: a modern plague // South Med J -2007. -№- P. 287-94.
- WHO European Centre for Environment and Health. Burden of Disease From Environmental Noise: Quantification of Healthy Life Years Lost in Europe // Copenhagen: Regional Office for Europe. - [displayed 20 October, 2014]. Available at http://www.euro.who.int/data/assets/pdf_file/0008/136466/e94888.pd.
- Harding A. H., Frost G. A., Tan E., Tsuchiya A., Mason H. M. The cost of hypertension-related ill-health attributable to environmental noise // Noise Health. – 2013. -№15. – Р. 437-45.
- World Health Organization (WHO). Prevention of noiseinduced hearing loss // WHO-PDH Informal Consultation Report. Geneva: WHO.-
- Babisch W. Updated exposure-response relationship between road traffic noise and coronary heart diseases: A meta-analysis // Noise Health. – 2014. - № 16. – Р. 1-9.
- Loomans E. M., van Dijk A. E. , Vrijkotte T. G., van Eijsden M., Stronks K., Gemke RJ, Van den Bergh BR. Psychosocial stress during pregnancy is related to adverse birth outcomes: results from a large multi-ethnic community-based birth cohort // Eur J Public Health. – 2013. - №23. –Р. 485-91.
- Littleton HL, Bye K, Buck K, Amacker A. Psychosocial stress during pregnancy and perinatal outcomes: a meta-analytic review // J Psychosom Obstet Gynaecol. – 2010. - №31. – Р.219-28.
- Spreng M. Central nervous system activation by noise // Noise Health. – 2000. -№2. – Р. 49-58.
- Ising H., Kruppa B. Health effects caused by noise: evidence in the literature from the past 25 years // Noise and Health. – 2004. -№22. – Р. 5-13.
- Babisch W. Epidemiological studies of the cardiovascular effects of occupational noise- a critical appraisal // Noise Health. – 1998. -№1. - Р. 24-39.
- Westman J. C., Walters J. Noise and stress: a comprehensive approach // Environ Health Perspect. – 1981. -№41. - Р. 291-309.
- Geber W. Developmental effects of chronic maternal audiovisual stress on the rat fetus // Embryol. Exp. Morphol. – 1966. - №16. – Р. 1-16.
- Geber W. Cardiovascular and teratogenic effects of chronic intermittent noise stress // In: Welch BL and Welch AS, eds. Physiological Effects of Noise, Plenum Press, New York. - –Р. 85-90.
- Wu T-N., Chen L-J., Lai J-S., et al. Prospective Study of Noise Exposure During Pregnancy on Birth Weight // Am J Epidemiol. – 1996. -№143(8). – Р. 792-6.
- de Weerth C., Buitelaar J. Physiological stress reactivity in human pregnancy--a review // Neurosci Biobehav Rev. – 2005. - №29. – Р. 295-312.
- Kalburova F. Other extra-auditory alterations, alterations in hearing sensitivity, correlations of auditory and extra-auditory alterations // In: Tzvetkov D, Angelova M, eds. Infrasound, ultrasound, noise and vibrations. 2nd ed. Sofia: Medicina i fizkultura. - – Р. 116-26 (in Bulgarian).
- Ando Y., Hattori H. Effects of noise on human placental lactogen (HPL) levels in maternal plasma // Br J Obstet Gynaecol. – 1977. - №84. – Р. 115-8.
- Querleu D., Renard X., Crépin G. Bruit intra-utérin et perceptions auditives du foetus. [Intra-uterine sound and fetal auditory perception] // Bulletin de l'Académie Nationale de Médecine. -1981. - №165(5). – Р. 581-8 (in French).
- Querleu D., Renard X., Versyp F., Paris-Delrue L., Crèpin G. Fetal hearing // Eur J Obstet Gynecol Reprod Biol. – 1988. - №28(3). – Р. 191-212.
- Szmeja Z., Słomko Z., Sikorski K., Sowiński H. The risk of hearing impairment in children from mothers exposed to noise during pregnancy // Int J Pediatr Otorhinolaryngol. -1979. - №1. – Р. 221-9.
- Gerhardt K. J., Abrams R. Fetal exposures to sound and vibroacoustic stimulation // J Perinatol. – 2000. - №20. – Р. S20–S29.
- Meyer R. E. , Aldrich T. E., Easterly C. Effects of noise and electromagnetic fields on reproductive outcomes // Environ Health Perspect. – 1989. - №81. – Р. 193-200.
- Hohmann C., Grabenhenrich L., de Kluizenaar Y., Tischer C., Heinrich J., Chen C. M., Thijs C., Nieuwenhuijsen M., Keil T. Health effects of chronic noise exposure in pregnancy and childhood: a systematic review initiated by ENRIECO // Int J Hyg Environ Health. – 2013. - №216. – Р. 217-29.
- Smith V., Devane D., Begley C. M., Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions // BMC Med Res Methodol. – 2011. – Р. 11:15.
- Bastian H., Glasziou P., Chalmers I. Seventy-five trials and eleven systematic reviews a day: how will we ever keep up // PLoS Medicine. – 2010. - №7. –
- Moher D., Tetzlaff J., Tricco A.C., Sampson M., Altman D. Epidemiology and reporting characteristics of systematic reviews // PLoS Medicine. – 2007. - №4. - e78.
- Pieper D., Buechter R., Jerinic P., Eikermann M. Overviews of reviews often have limited rigor: a systematic review // J Clin Epidemiol. – 2012. - №65 – Р. 1267-73.
- Shea B. J., Hamel C., Wells G.A., Bouter L.M., Kristjansson E., Grimshaw J., Henry D.A., Boers M. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews // J Clin Epidemiol. – 2009. - №62. – Р. 1013-20.
- Pieper D., Mathes T., Eikermann M. Can AMSTAR also be applied to systematic reviews of non-randomized studies? // BMC Res Notes. – 2014.- №7. – Р.
- Jadad A. R., Cook D. J., Browman G. A guide to interpreting discordant systematic reviews // CMAJ. – 1997. - №156. – Р. 1411-6.
- Pieper D., Antoine S. L., Mathes T., Neugebauer E. A., Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview // J Clin Epidemiol. – 2014. - №67 – Р. 368-75.
- Effets du bruit en milieu de travail durant la grossesse: synthèse systématique avec méta-analyse et méta-régression [Effects of noise in the workplace during pregnancy: systematic review with meta-analysis and meta-regression]. // Gouvernement du Quebec, Ministeres des Communications. - 2009 (in French). [displayed 20 October, 2014]. Available at http://www.inspq.qc.ca/pdf/publications/1040_BruitTravailGrossesseSynthese.pdf.
- Dzhambov A. M., Dimitrova D. D., Dimitrakova E. Noise Exposure during Pregnancy, Birth Outcomes and Fetal Development: Meta-Analyses Using Quality Effects Model. Fol Med (Plovdiv). – 2014. - №56. – Р. 204-14.
- Ristovska G., Laszlo H. E., Hansell A. Reproductive outcomes associated with noise exposure - a systematic review of the literature // Int J Environ Res Public Health. – 2014. – 11. – Р. 7931-52.
- Bastos M. A., Duarte S.C.A., Araújo R. M. S., Ramalho C., Torres da Costa J. Occupational noise exposure during pregnancy: a systematic review // In: Eds. Arezes P, Baptista JS, Barroso MP, Carneiro P, Cordeiro P, Costa N, Melo RB, Miguel SA, Perestrelo G, eds. Occupational Safety and Hygiene II. London, CRC Press. - –Р. 793-9.
- Minozzi S., Pistotti V., Forni M. Searching for rehabilitation articles on MEDLINE and EMBASE. An example with cross-over design // Arch Phys Med Rehabil. – 2000. -№81. – Р. 720–2.
- Woods D., Trewheellar K. MEDLINE and EMBASE complement each other in literature searches // BMJ. – 1998. -№316. – Р.
- Suarez-Almazor M. E., Belseck E., Homik J., Dorgan M., Ramos-Remus C. Identifying clinical trials in the medical literature with electronic databases: MEDLINE alone is not enough // Control Clin Trials. – 2000. -№21. – Р. 476–87.
- McDonald A. D., McDonald J. C., Armstrong B., Cherry N. M., Côté R., Lavoie J., Nolin A. D., Robert D. Fetal death and work in pregnancy // Br J Ind Med. – 1988. - №45. – Р. 148-57.
- Hartikainen-Sorri A. L., Sorri M., Anttonen H. P., Tuimala R., Läärä E. Occupational noise exposure during pregnancy: a case control study // Int Arch Occup Environ Health. – 1988. -№60. – Р. 279-83.
- Nurminen T., Kurppa K. Occupational noise exposure and course of pregnancy // Scand J Work Environ Health. – 1989. - №15. – Р. 117–24.
- Kurppa K., Rantala K., Nurminen T., Holmberg P. C., Starck J. Noise exposure during pregnancy and selected structural malformations in infants // Scand J Work Environ Health. – 1989. - №15. – Р. 111–6.
- Zhang J., Cai W. W., Lee D. Occupational hazards and pregnancy outcomes // Am J Ind Med. – 1992. - №21. – Р. 397-408.
- Hruba D., Kukla L., Tyrlik M. Occupational risks for human reproduction: ELSPAC Study European Longitudinal Study of Pregnancy and Childhood // Cent Eur J Public Health. – 1999. - №7. – Р. 210-5.
- Hartikainen A. L., Sorri M., Anttonen H., Tuimala R., Läärä E. Effect of occupational noise on the course and outcome of pregnancy // J. Work Environ. Health. – 1994. - №20. – Р. 444-50.
- Magann E. F., Evans S. F., Chauhan S. P., Nolan T. E., Henderson J., Klausen J. H., Newnham J. P., Morrison J. The effects of standing, lifting and noise exposure on preterm birth, growth restriction, and perinatal death in healthy low-risk working military women // J Matern Fetal Neonatal Med. – 2005. - №18. – Р. 155–62.
- Knipschild P., Meijer H., Salle H. Aircraft noise and birth weight // Int Arch Occup Environ Health. – 1981. - №48. – Р. 131-6.
- McDonald A. D., Armstrong B., Cherry N. M., Delorme C., Diodati-Nolin A., McDonald J. C., Robert D. Spontaneous abortion and occupation // J Occup Med. – 1986. - №28. – Р. 1232-8.
- Luke B., Mamelle N., Keith L., Munoz F., Minogue J., Papiernik E., Johnson T. The association between occupational factors and preterm birth: a United States nurses' study. Research Committee of the Association of Women's Health, Obstetric, and Neonatal Nurses // Am J Obstet Gynecol. – 1995. - №173. – Р. 849-62.
- Saurel-Cubizolles M. J., Zeitlin J., Lelong N., Papiernik E., Di Renzo G. C., Bréart G.; Europop Group. Employment, working conditions, and preterm birth: results from the Europop casecontrol survey // J Epidemiol Community Health. – 2004. - №58. – Р. 395-401.
- Croteau A., Marcoux S., Brisson C. Work activity in pregnancy, preventive measures, and the risk of delivering a small-for-gestational-age infant // Am J Public Health. – 2006. - №96. – Р. 846-55.
- Haelterman E., Marcoux S., Croteau A., Dramaix M. Population-based study on occupational risk factors for preeclampsia and gestational hypertension // Scand J Work Environ Health. – 2007. - №33. – Р. 304–17.
- Chen D., Cho S., Chen C., Wang X., Damokosh A. I., Ryan L., Smith T. J., Christiani D. C., Xu X. Exposure to benzene, occupational stress, and reduced birth weight // Occup Environ Med. – 2000. - №57. – Р. 661-7.
- Schell L. Environmental noise and human prenatal growth // Am. J. Phys. Anthropol. – 1981. - №56. – Р. 63-70.
- Peoples-Sheps M. D., Siegel E., Suchindran C. M., et al. Characteristics of maternal employment during pregnancy: effects on low birth weight // Am J Public Health. – 1991. - №81. – Р. 1007-12.
- Hanke W., Kalinka J., Makowiec-Dabrowska T., Sobala W. Heavy physical work during pregnancy--a risk factor for small-for-gestational-age babies in Poland // Am J Ind Med. – 1999. - №36. – Р. 200-5.
- McDonald A., Sloan M., Armstrong B. Noise at work and the outcome of pregnancy. In: Sakurai H, Okazari I, Omae K, eds. The Seventh International Symposium on Epidemiology in Occupational Health. Elsevier Science Publishers B.V. – 1990. - №889. – Р. 297-300.
- Mamelle N., Laumon B., Lazar P. Prematurity and occupational activity during pregnancy // Am J Epidemiolл – 1984. - №119. – Р. 309–22.
- Croteau A., Marcoux S., Brisson C. Work activity in pregnancy, preventive measures, and the risk of preterm delivery // Am J Epidemiol. -2007. - №166. – Р. 951-65.
- Saurel-Cubizolles M. J., Kaminski M., Du Mazaubrun C., Breart G. Les conditions de travail professionnel des femmes et l'hypertension artérielle en cours de grossesse [Working conditions of women with arterial hypertension during pregnancy] // Rev Epidemiol Sante Publique. – 1991. - №39(1). – Р. 37-43. PMID: 2031095. (in French)
- Irwin D. E., Savitz D. A., St André K. A., Hertz-Picciotto I. Study of occupational risk factors for pregnancy-induced hypertension among active duty enlisted Navy personnel // Am J Ind Med. – 1994. - №25. – Р. 349-59.
- McDonald A. D., McDonald J. C., Armstrong B., Cherry N. M., Nolin A. D., Robert D. Prematurity and work in pregnancy // Br J Ind Med. – 1988. - №45. – Р. 56-62.
- Florack E. I., Zielhuis G. A., Pellegrino J. E., Rolland R. Occupational physical activity and the occurrence of spontaneous abortion // Int J Epidemiol. -1993. - №22. – Р. 878-84.
- Hansteen I. L., Kjuus H., Fandrem S. Spontaneous Abortions of Known Karyotype Related to Occupational and Environmental Factors: A Case-Referent Study // Int J Occup Environ Health. – 1996. - №2. – Р. 195-203.
- Wergeland E., Strand K. Working conditions and prevalence of pre-eclampsia, Norway 1989 // Int J Gynaecol Obstet. – 1997. - №58. – Р. 189-96.
- Zhan C., Lu Y., Li C., Wu Z., Long Y., Zhou L., Zhou B. A study of textile noise influence on maternal function and embryo-growth // Hua Xi Yi Ke Da Xue Xue Bao. – 1991. - №22. – Р. 394-8. (in Chinese)
- Gehring U., Tamburic L., Sbihi H., Davies H. W., Brauer M. Impact of noise and air pollution on pregnancy outcomes // Epidemiology. – 2014. - №25. – Р. 351-8.
- Jones F. N., Tauscher J. Residence under an airport landing pattern as a factor in teratism // Arch Environ Health. – 1978. - №33. – Р. 10-12.
- Kurppa K., Holmberg P. C., Hernberg S., Rantala K., Riala R., Nurminen T. Screening for occupational exposures and congenital malformations // Scand J Work Environ Health. – 1983. - №9. – Р. 89-93.
- Nurminen T. Shift work, fetal development and course of pregnancy // Scand J Work Environ Health. – 1989. - №15. – Р. 395-403.
- Wang Y., Liu Y., Dai Y. A 1:2 matched case-control study on risk factors of unexplained recurrent spontaneous abortion // Chin J Prev Control Chronic Dis. – 2011. - №19. – Р. 49–51.
- Edmonds L. D., Layde P. M., Erickson J. Airport noise and teratogenesis // Arch Environ Health. – 1979. - №34. – Р. 243-7.
- Matsui T., Matsuno T., Ashimine K., Miyakita T., Hiramatsu K., Yamamoto T. Association between the rates of low birth-weight and/or preterm infants and aircraft noise exposure // Nihon Eiseigaku Zasshi. – 2003. - №58. – Р. 385-94.
- Ando Y., Hattori H. Statistical studies on the effects of intense noise during human fetal life // J Sound Vib. – 1973. - №27. – Р. 101-10.
- Bendokiene I., Grazuleviciene R., Dedele A. Risk of hypertension related to road traffic noise among reproductive-age women // Noise Health. - 2011. - №13. – Р. 371-7.
- Well G. A., Shea B., O’Connell D., Peterson J., Welch V., Losos M., Tugwell P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. [displayed 20 October, 2014]. Available at http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- Doi S. Evidence Synthesis for Medical Decision Making and the Appropriate Use of Quality Scores // Clin Med Res. - 2014 (in press).
- Nieuwenhuijsen M. J., Dadvand P., Grellier J., Martinez D., Vrijheid M. Environmental risk factors of pregnancy outcomes: a summary of recent meta-analyses of epidemiological studies // Environ Health. – 2013. - Р. 12:6.
- Pieper D., Mathes T., Neugebauer E., Eikermann M. State of evidence on the relationship between high-volume hospitals and outcomes in surgery: a systematic review of systematic reviews // J Am Coll Surg. – 2013. - №216. – Р. 1015-25.e18.
- Yaffe J., Montgomery P., Hopewell S., Shepard L. Empty Reviews: A Description and Consideration of Cochrane Systematic Reviews with No Included Studies. PLoS ONE. – 2012 . -№7. – Р. e36626.
- Rini C. K., Dunkel-Schetter C., Wadhwa P. D., Sandman C. Psychological adaptation and birth outcomes: the role of personal resources, stress, and sociocultural context in pregnancy // Health Psychol. – 1999. - №18. – Р. 333-45.
- American College of Obstetricians and Gynecologists Committee on Health Care for Undeserved Women. ACOG Committee on Health Care for Underserved Women. Psychosocial risk factors: perinatal screening and intervention // Obstet Gynecol. – 2006. - №108. – Р. 469-77.