ВЛИЯНИЕ ТРАДИЦИОННОЙ КАРДИО-НЕФРОПРОТЕКТИВНОЙ ТЕРАПИИ НА МАРКЕРЫ СЕРДЕЧНО-СОСУДИСТОГО РИСКА (FGF-23, KLOTHO) У ПАЦИЕНТОВ С ХРОНИЧЕСКОЙ БОЛЕЗНЬЮ ПОЧЕК
Милованова Л.Ю.1, Козловская Л.В.2, Милованова С.Ю.3, Маркина М.М.4, Милованов Ю.С.5, Плотникова А.А.6, Фомин В.В.7, Мухин Н.А.8, Снитцар С.В.9, Лебедева М.В.10, Бекетов В.Д.11
1Кандидат медицинских наук, доцент кафедры, 2Доктор медицинских наук, профессор, 3Доктор медицинских наук, ведущий научный сотрудник, 4Аспирант, 5Доктор медицинских наук, профессор, 6Кандидат медицинских наук, 7Доктор медицинских наук, профессор, 8Доктор медицинских наук, профессор, академик РАН, 9Студент, 10Кандидат медицинских наук, доцент, 11Аспирант, Первый Московский Государственный Медицинский Унивеситет им. И.М.Сеченова, Кафедра внутренних, профессиональных болезней и пульмонологии, Кафедра нефрологии и гемодиализа, Клиника нефрологии, внутренних и профессиональных болезней, Россия.
Работа выполнена при поддержке Российского Научного Фонда (грант № 14-15-00947 2014 г.)
ВЛИЯНИЕ ТРАДИЦИОННОЙ КАРДИО-НЕФРОПРОТЕКТИВНОЙ ТЕРАПИИ НА МАРКЕРЫ СЕРДЕЧНО-СОСУДИСТОГО РИСКА (FGF-23, KLOTHO) У ПАЦИЕНТОВ С ХРОНИЧЕСКОЙ БОЛЕЗНЬЮ ПОЧЕК
Аннотация
Целью исследования являлось определить влияние традиционной кардио-нефропротективной терапии на сывороточные маркеры сердечно-сосудистого риска (FGF-23, Klotho) у пациентов с хронической болезнью почек (ХБП). Результаты исследования свидетельствуют о возможности практического использования FGF-23 и Klotho в качестве ранних диагностических маркеров сердечно-сосудистого риска, а также о том, что адекватная коррекция этих изменений, начатая на предиализных стадиях ХБП, может позволить снизить риск сердечно-сосудистых осложнений и повысить выживаемость пациентов с ХБП в целом.
Ключевые слова: хроническая болезнь почек, FGF-23, Klotho, кардио-нефропротективная терапия
Milovanova L.Y.1, Kozlovscaya L.V.2, Milovanova S.Y.3, Markina M.M.4, Milovanov Y.S.5, Plotnikova A.A.,6 Fomin V.V.7, Mukhin N.A.8, Snitcar S.V.,9 Lebedeva M.V.10, Beketov V.D.11
1PhD in medicine, associate professor, 2Рrofessor, 3Doctor of Medical Sciences, 4Postgraduate student, 5Professor, 6PhD in medicine, 7Professor, 8Professor, 9Student, 10PhD in medicine, associate professor, 11Postgraduate student, First Moscow State Medical University named after I.M. Sechenov, Department of internal, occupational diseases and pulmonology, Department of nephrology and hemodialysis, Сlinic of nephrology, internal and occupational disease, Russia.
This work was supported by the Russian Science Foundation (grant № 14-15-00947 2014 year)
INFLUENCE OF TRADITIONAL CARDIO-NEPHROPROTECTIVE THERAPY ON CARDIOVASCULAR RISK MARKERS (FGF-23, KLOTHO) IN PATIENTS WITH CHRONIC KIDNEY DISEASE
Abstract
The aim of the study was to evaluate the influence of the traditional cardio-nephroprotective therapy on serum markers of cardiovascular risk (FGF-23, Klotho) in patients with chronic kidney disease (CKD).The study showed the possibility of practical use of FGF-23 and Klotho as an early diagnostic marker of cardiovascular risk and that adequate correction of their changes started in predialysis CKD can be initiated to reduce the risk of cardiovascular complications and increase the survival of patients with CKD in general.
Keywords: chronic kidney disease, FGF-23, Klotho, the traditional cardio-nephroprotective therapy
Chronic renal failure (chronic kidney disease - CKD stages III-VD) spreads widely in population (10-15% of a population), characterized by a high rate of cardiovascular events (CVE) [1-3], the risk of which, including young people, increases 100 and more times [4].
In the genesis of CVE in CKD many mechanisms have a value. Among them, in recent years the dysfunction of morphogenetic proteins (FGF-23 and Klotho) plays а growing role. According to Gutierrez O.M. et al. [5], high levels of FGF-23 correlate with an increase in the left ventricular mass index (LVMI). Klotho gene damage in experimental mice causes an ectopic calcification, pathological fractures, premature aging [6,8]. On the other hand, the circulating form of Klotho protein can function as a humoral factor that protects the cardiovascular system [7,9]. Overexpression of the Klotho protein provides both renal and cardiovascular protection [9, 10].
Most studies of morphogenetic proteins were connected with an investigation of the cardiorenal relationships of these markers and today their role in the development of cardiovascular complications in patients with chronic kidney disease quite clearly defined. At the same time, there is no publication dial with the impact of treatment to these factors in CKD patients.
Materials and Methods: 130 patients with CKD I-VD stage were included in the study: 30-with chronic glomerulonephritis, 23-chronic tubulointerstitial nephritis, 28-hypertensive nephrosclerosis, 22-multicystic kidney disease, 27- type II diabetes (64 men and 66 women, aged 20-65 years, mean age at enrollment was 41 ± 6,7 years).Serum FGF-23 levels (Human FGF-23 ELISA kit using monoclonal antibodies to the full FGF-23 molecule), Klotho (Human alpha-Kl ELISA). To evaluate the effect of therapy, patients were divided into groups: 1- CKD I-IIIA st, 2- CKD IIIB-IV st and 3- CKD V-VD st .
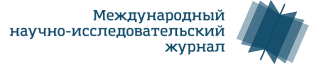
Results: In group 1, we evaluated the effects of antihypertensive therapy. The highest Klotho levels were observed in patients, whose target values of blood pressure were achieved with the help of angiotensin receptor blockers and angiotensin converting enzyme inhibitors (ACE) compared with those who used other groups of drugs or unreached target blood pressure levels (р<0,01) (fig. 1)
Fig. 1. The effects of antihypertensive therapy to serum levels of Klotho in 1-st group patients, who reached target blood pressure levels.
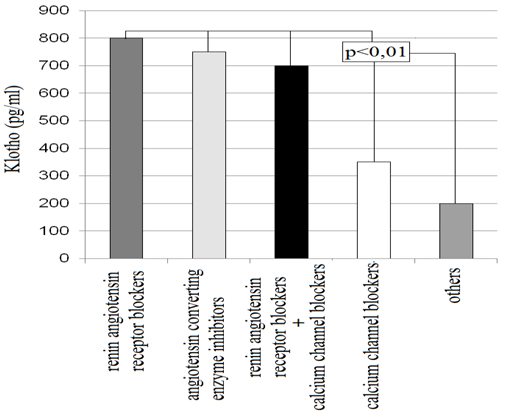
In group 2 it was evaluated the effects of low-protein diet with low phosphate content (< 800 mg/day) in combination with keto / amino acids drug (Ketosteril) . It was shown that patients used a low-protein diet with low phosphate content, balanced amino / keto acids, had higher Klotho and lower FGF-23 levels (р<0,05 and р<0,01 respectively) (fig. 2).
Fig. 2. The effects of low-protein diet with low phosphate content (< 800 mg/day) in combination with keto / amino acids drug (Ketosteril) in serum FGF-23 and Klotho levels in CKD patients.
Patients from the 2nd and 3rd groups, who used low phosphate diet in combination with phosphate binders (calcium carbonate, renagel) to reduce the level of serum phosphate and reached the target serum level of phosphate (serum phosphorus less than 1.62 mmol / L) serum FGF- 23 and PTH were statistically lower than that in patients with elevated phosphate levels (р<0,01 and p<0,01 respectively).
Patients from the 2nd and 3rd groups who used to reduce the level of PTH selective activators of vit D receptors –VDR- (zemplar) recorded higher levels of Klotho in serum as compared with patients who use non-selective VDR (р<0,01).
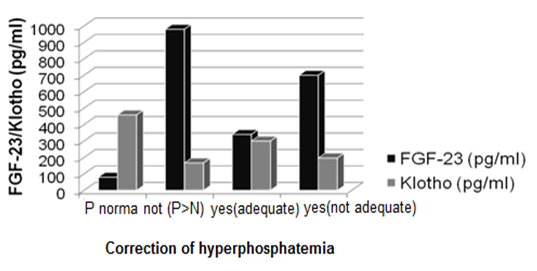
In addition, patients 2-nd and 3-rd groups who achieved and maintain target Hb level (120 g / l) with help of erythropoiesis stimulating agents (ESA) + iron intravenously also had higher Klotho levels than patients who drugs to improve Hb used irregularly and who remained of anemia (Hb <120 g / l; р<0,01) (fig. 3).
Fig. 3. The effect of anemia correction on serum Klotho levels in 2nd and 3rd groups patients
At the same time it was shown that predialysis patients with corrected serum levels of FGF-23 and Klotho have lower cardiovascular complications risk (RR= 0,95 versus 1,10, 95% DI; р<0,01), need for hospitalization ( r=0,457; р<0,01 ) and better survival during the first year of hemodialysis.
Conclusion: The study showed the possibility of practical use of FGF-23 and Klotho as an early diagnostic marker of cardiovascular risk and that adequate correction of their changes started in predialysis CKD can be initiated to reduce the risk of cardiovascular complications and increase the survival of patients with CKD in general.
References
- Couser WG.,Remuzzi G., Mendis S.et al. The contribution of chronic kidney disease to the global burden of major noncommunicable diseases// Kidney int. 2011. Vol. 80, № 12. P. 1258-1270
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO clinical practice guideline for the diagnosis, evalution, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD)// Kidney Int. 2009. Vol. 76, Suppl.113.P. 1-130
- Milovanova L., Milovanov Y., Plotnikova A. Phosphorus and Calcium Metabolism Disorders Assosiated with Chronic Kidney Disease Stage III-IV (Systematic Rewiew and Meta-Analysis)// In: Chronic Kidney Disease and renal Transplantation.- Croatia.: INTECH, 2012.-P. 95-118
- Kuo-Cheng Lu, Chia-Chao Wu, Jen-Fen Yen et al. Vascular calcification and Renal Bone Disorders// Scientific World Journal. 2014. Published online 2014 Jul 17. doi: 10.1155/2014/637065
- Gutierrez O.M., Januzzi J.L., Isacova T, et al. Fibroblast growth factor-23 and left ventricular hypertrophy in chronic kidney disease// Circulation. 2009. Vol.119, № 9.P. 2545-2552
- Hu M.C., Shi M., Zhang J. et al. Klotho deficiency causes vascular calcification in chronic kidney disease// Am. J. Soc. Nephrol. 2011. Vol 1, № 1. P. 124-136
- Milovanova L.Y., Milovanov Y.S., Kozlovskaya L.V. Nephro-cardioprotective role of the circulating forms of the KLOTHO protein in chronic kidney disease// Clinical Nephrology. - 2013. - № 3.- Р. 7-10
- Kuro-o M. Klotho in chronic kidney disease—What's new?// Nephrology Dialysis Transplant. 2009. Vol. 24, №58. P. 1705-1708
- Ming Chang Hu, Makoto Kuro-o, Orson W. Moe Klotho and Chronic Kidney Disease// Contrib Nephrol. 2013. №18, P. 47–63.
- Ming Chang Hu, Makoto Kuro-o, Orson W. Moe RENAL AND EXTRA-RENAL ACTIONS OF KLOTHO// Semin Nephrol. 2013.Vol. 33, № 2. P. 118–129