АКТИВНОСТЬ МАРКЕРОВ АПОПТОЗА ПРИ HPV-АССОЦИИРОВАННЫХ ПАТОЛОГИЯХ ШЕЙКИ МАТКИ
АКТИВНОСТЬ МАРКЕРОВ АПОПТОЗА ПРИ HPV-АССОЦИИРОВАННЫХ ПАТОЛОГИЯХ ШЕЙКИ МАТКИ
Научная статья
Виноградова О.П.1, *, Орлова Е.А.2, Артемова О.И.3, Епифанова О.В.4, Андреева Н.А.5
1, 2, 4 Пензенский институт усовершенствования врачей – филиал Российской медицинской академии последипломного образования Минздрава России, Пенза, Россия;
3 Пензенский государственный университет, Пенза, Россия;
5 Национальный исследовательский Мордовский государственный университет имени Н.П. Огарёва, Саранск, Россия
* Корреспондирующий автор (o_vinogradova69[at]mail.ru)
АннотацияРак шейки матки (РШМ) является одним из лидеров онкологических заболеваний среди женского населения, что остается важной социальной проблемой. При исследовании процессов канцерогенеза было установлено, что формировании атипических изменений сопровождается замедлением программированной клеточной гибели, то есть происходит торможение апоптоза. Возможно, на начальных этапах формирования цервикальных поражений при воздействии вируса папилломы человека (ВПЧ), а именно при цервикальных интраэпителиальных поражениях 1 степени, так же происходит влияние на апоптотические механизмы.
Ключевые слова: цервикальная дисплазия, каспаза-1, каспаза-3, каспаза-9, ВПЧ.
ACTIVITY OF APOPTOSIS MARKERS IN HPV-ASSOCIATED CERVICAL PATHOLOGIES
Research article
Vinogradova O.P.1, *, Orlova E.A.2, Artemova O.I.3, Epifanova O.V.4, Andreeva N.A.5
1, 2, 4 Branch of Russian Medical Academy of Postgraduate Education of the Ministry of Healthcare of the Russian Federation, Penza, Russia;
3 Penza State University, Penza, Russia;
5 National Research Ogarev Mordovia State University, Saransk, Russia
* Corresponding author (o_vinogradova69[at]mail.ru)
AbstractCervical cancer (CC) is one of the leaders of oncological diseases among the female population, which remains an important social problem. When studying the processes of carcinogenesis, it was found that the formation of atypical changes is accompanied by a slowdown in programmed cell death, that is, inhibition of apoptosis. It is possible that at the initial stages of the formation of cervical lesions under the influence of the human papillomavirus (HPV), namely with cervical intraepithelial lesions of the 1st degree, the effect on apoptotic mechanisms also occurs.
Keywords: ectocervical dysplasia, caspase-1, caspase-3, caspase-9, HPV. IntroductionDespite numerous studies, diagnostic criteria and treatment options, the general pathology of gynecological morbidity includes pathologies of the cervix [1]. Currently, the most urgent problem in the field of obstetrics and gynecology is the combination of changes in the cervix with the activity of the human papillomavirus (HPV), with a frequent outcome in malignancy. Various types of HPV are diagnosed in 97% of confirmed cervical cancers [4]. Relatively recently, the world health organization introduced screening programs aimed at the earliest possible diagnosis of pathological changes in the cervix against the background of HPV [1], [2], [5]. With the progression of the pathology of the cervical zone, HPV DNA is introduced into the cell genome [7], [9], [13], thereby provoking proliferation processes [8], [10], [21]. However, it is not fully understood at what stage the virus influences the cellular genome and what causes the cell to change its natural processes, for example, apoptosis. It was found that during the formation of cervical cancer, there is a decrease in the activity of apoptotic mechanisms, where the leading role is given to caspases, the main enzymes [6], [15], [18], [19]. Therefore, the formation of the correct tactics for managing patients based on the activity of apoptosis markers is the basis for effective preventive measures for cervical cancer.
The aim of the study was to study the role of caspase-1, caspase-3 and caspase-9 in the formation of cervical intraepithelial neoplasia I (CIN I) by determining the levels of these markers in the epithelial cells of the cervical zone in HPV-positive patients of fertile age.
Materials and Research methods
For the study, 95 women were selected at the age from 18 to 45 years. The main study group included 55 patients with mild cervical intraepithelial neoplasia associated with human papillomavirus. The control group consisted of 40 healthy women.
When working with patients, all the requirements for medical research at universities in the Russian Federation were observed.
In the period from 2018 to 2019, a study was conducted of 95 women who applied for an outpatient clinic in Penza. In order to search for new approaches to the treatment of human papillomavirus infection, the factors of the cytokine response and markers of apoptosis in CIN I degree against the background of papillomavirus infection were assessed and their changes were analyzed in comparison with conventionally healthy women with normal findings of an oncocytological smear from the cervix without HPV. The criteria for inclusion in the groups with pathological conditions of the cervix were: the presence of high-risk HPV virus replication in the cervical canal, established by polymerase chain reaction (PCR); CIN I, histologically confirmed; absence in the last 6 months before the start of the study of therapy with drugs that could affect the results of the study; adequate contraception for women of childbearing age (using a barrier method of contraception); written informed voluntary consent to participate in the study; transformation zone 1 or 2 type; “Normocenosis” based on the results of the assessment of the lower part of the gynecological tract; patient compliance. The exclusion criteria were: age under 18 and over 45; pregnancy, lactation; severe somatic pathology; taking medications that could affect the studied parameters; the presence of decompensated diseases or acute conditions, including concomitant mental illness; the presence of other sexually transmitted infections; inability to follow the terms of the protocol.
In order to assess the cellular composition and detect the presence of atypical epithelial cells, a cytological examination of smears from the cervix of the examined women was carried out. The material for cytological examination was scraping from the cervical canal, transformation zone and from the surface of the cervix, obtained using a disposable cervical brush. The staining of cervical smears was performed according to the Pap test. The evaluation of the results of the cytological study was carried out in accordance with the general provisions of the Bethesda Informative Classification System (The Bethesda System), developed in the USA in 1988.
All patients underwent colposcopy to assess the state of the cervix. If atypical changes were detected, a multifocal biopsy was performed to establish a histological diagnosis. All results were documented and recorded graphically.
The detection and differentiation of DNA of human papillomaviruses was carried out by PCR with hybridization fluorescence detection "AmpliSens® HPV VKR screen-titer-FL", according to the recommendations of the manufacturer FBSI "TsNIIE" Rospotrebnadzor (Moscow). The reagent kit is intended for the detection and quantitative determination of HPV DNA of high carcinogenic risk (HRS) of 16,18,31,33,35,39,45,51,52,56,58,59 types in clinical material. The method is based on the simultaneous amplification of HPV DNA regions and a DNA region of the β-globin gene, which was used as an endogenous internal control, with hybridization-fluorescent endpoint detection (FEP format). Scraping discharge of the cervical canal was used as a material for PCR diagnostics.
To determine the expression of the level of caspase 1, caspase 3 and caspase 9, we used an enzyme-linked immunosorbent assay with a set of reagents from Cloud.corp., the level of the studied caspases was assessed by the sandwich method for tissue homongenates.
Statistical processing of indicators was carried out using assessment methods and using the STATISTICA 9.0 program. Descriptive statistics were also used in the processing of the obtained data. When carrying out statistical indicators, the Fisher method was used - the method of angular transformation. The difference between the compared data was considered significant at P> 0.05.
Results and DiscussionAccording to the results of the research during the observation, the examined women were divided into groups. Among all examined patients, 55 women were verified to have HPV-positive cervical intraepithelial lesion of the 1st degree. They made up research group. The remaining 40 women with a normal cytological picture did not have HPV and, accordingly, had the NILM category according to oncocytology. The last group of patients constituted the control group. Examination of this group made it possible to obtain the results of the physiological norm of the studied parameters. The age of the examined women varied from 19 to 45 years. So the average age in the research group of women with CIN I was 27.05 ± 0.51, in the control group 30.41 ± 1.07.
The first stage was a cytological examination of the patients. In the control group, 40 patients in the cytological protocol had a NILM conclusion (100%).
In analyzing the data of cytological examination in research group 38 patients (69%) had normal results, 15% (8 patients) had low-grade squamous intraepithelial lesion (LSIL), and HSIL was found in 16% (9 patients). This diagnostic method is a screening method and makes it possible to identify women at risk of developing neoplasia and cervical cancer. Taking into account the sensitivity and specificity of the cytological research method (no more than 60%) (4, 8), then when interpreting the results of cytology, 49.5% of false-positive results were obtained.
To determine the nature of the lesions of the cervical zone, an extended colposcopic examination was carried out. The main criterion for inclusion in the study was the presence of a type I or II transformation zone, which made it possible to fully assess the state of the cervix. All HPV positive patients with CIN I were diagnosed with an abnormal colposcopic picture. Mild lesions (grade I) on the cervix were diagnosed in 36 patients, which was 65%, and severe lesions (grade II) - in 19 patients (35%). Since, according to the clinical guidelines of november 2020 on cervical pathology, colposcopic examination is not final in the diagnosis, however, the results of colposcopy make it possible to identify areas for a multifocal biopsy of the cervix.
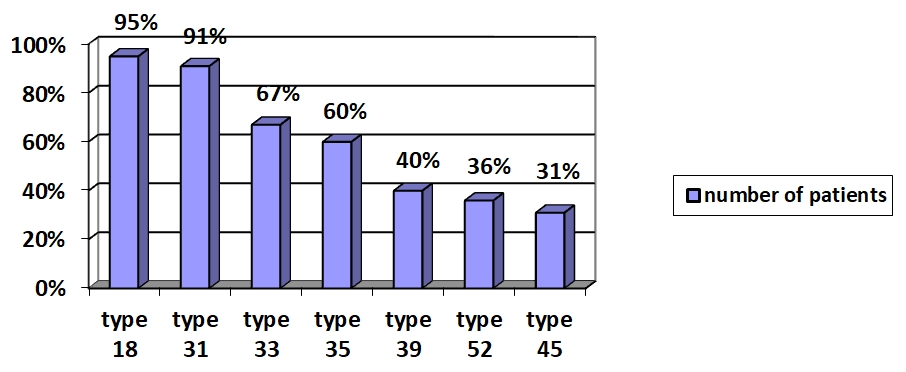
When analyzing the studied parameter, it was found that all patients with CIN I had combinations of several types of HPV and a clinically significant viral load (3-5 lg, > 5 lg) (fig.1).
Fig. 1 – Distribution of patients by HPV type
To establish a final diagnosis, a multifocal cervical biopsy with a histological examination was performed. The results of this histological examination served as the basis for the formation of research group: 55 patients (100%) conclusion on the result of histology CIN I.
The final stage in the diagnosis according to the clinical guidelines for cervical pathologies from 2020 is the histological examination, which served as the basis for the formation of the research group.
To determine the severity degree of the cervical changes and to evaluate the risk of developing atypical processes, an assessment of apoptotic process in the cervical mucus obtained during the cytological intake of the material was carried out. Determination of the level of caspase-1, caspase-3 and caspase-9 (Table 1) was another stage of the research.
Table 1 – The level of caspases in research groups
| Indicator | Caspase 1 Level, ng/ml | Caspase 3 Level, ng/ml | Caspase 9 Level, ng/ml |
| Control group, n = 40 | 0,060±0,01 | 0,188±0,04 | 0,213±0,03 |
| Research group , n = 55 | 0,062±0,03 | 2,772 ±0,03* | 2,311 ±0,05* |
Note: the assessment of the statistical significance of changes in the activity of caspase 3, caspase 9 and caspase 9 was carried out in accordance with the Wilcoxon-Mann-Whitney criteria. The symbol * marks the groups in which the caspase activity significantly differs from the “control” group (the differences are considered significant with p < 0,05)
Since the formation of dysplasia is the result of a violation of the natural balance between the processes of proliferation and cell death (apoptosis), the available data on the study of various mechanisms of the formation of resistance of tumor cells to apoptotic factors are ultimately aimed at suppressing the activity of these processes. In this regard, it is important to study the relationship between these indicators and parameters characteristic of dysplasia of the 1st severity [6], [11], [12], [14].
The caspase 1 values in the study group I were equal to 0,062 ± 0,03 ng / ml, and did not differ statistically from the control group, that is, they were at the limit of the method's sensitivity. Since caspase 1 plays a leading role in the activation of the inflammatory response, the data obtained make it possible to conclude that patients with CIN I lack an inflammatory component in the formation of pathological changes in the cervix.
In clinical conditions, an assessment of violation degree of the apoptotic program in HPV-associated cervical pathology by determining caspase-3 and caspase-9 expression was carried out. Studying effector caspase-3 and caspase-9, changes were obtained characterizing the progression degree of HPV presence in cervical epithelial cells. Due to the lack of normal values for caspase under study, the results in the immunological control group were taken as normal indicators. In research groups, the activity of effector caspase-3 and caspase-9 was higher relative to the control level, and increased as cervical pathology progressed against the background of the virus. These results confirm the formation of apoptosis resistant process in HPV-affected cells [9], [11], [12], [21] due to activation of caspase genes in changed areas of the cervical zone. It supplements the previous studies confirming the data on atypical progression with CIN III in cervical cancer, and an increase in caspase-3 level and caspase-9 level [13], [15].
An increase in the severity of the pathological process in the cervix may be accompanied by the expression of caspase-3 and caspase-9 (Table 1). Perhaps this is due to the fact that this is explained by the fact that there are inactive monomeric precursors in the caspase cells, requiring cleavage of proenzyme and subsequent dimerization for activation. The implementation of these reactions is possible with successive mutual activation of caspases. The starting moment for such transformations is DNA damage, which in turn launches a caspase cascade. It can follow either external or internal pathway, but no matter what pathway the cascade is launched, caspase-3 and caspase-9 is its effector caspases. In this way, the mechanisms for HPV-associated cervical pathologies formation, such as CIN I, can be considered as expression of effector caspase-3 and caspase-9 levels. The studied cysteine protease is able to increase with introduction of HPV DNA into the host cell. Determination results of caspase-3 and caspase-9 have shown different values in the expression level of apoptosis marker in the cervical epithelium as HPV-associated pathology progresses, both in the control group and in the group with CIN I.
Determining the level of caspase-3 and caspase-9 in case of CIN I proves the validity of an in-depth dispensary observation: since, according to the literature, the reliability of the cytological study is no more than 60% (which is also confirmed in the research group) and eventual active treatment of these patients. The obtained data on changes in the apoptosis program and, as a consequence, local immunity are the pathogenetic rationale for a more in-depth and attentive approach to clinical examination of the female population.
ConclusionThe values of caspase 1 in the group of HPV-positive patients with CIN were at the limit of the sensitivity of the method and did not statistically differ from the control group. According to the literature data, caspase 1 plays a key role in the initiation of the inflammatory process, therefore, the obtained indicators allow us to conclude that there is no inflammatory component in epithelial cells in the formed research group.
The values of caspase 3 and caspase 9 in the study group were higher than in the control group, which may indicate the effect of the virus on the processes of apoptosis. An increase in the level of caspase 9 is possibly associated with participation in the internal, mitochondrial pathway, due to activation after the release of the apoptosome and the removal of antiapoptotic blocks from mitochondrial complexes [10], [12], [16].
Taking into account the peculiarity of caspase 3 to lead to total death of all cells, it, being the final link of the external pathway, closes the cascade of reactions, the launch of which begins with the influence of a trigger [13], [20], that is, possibly under the influence of HPV.
| Конфликт интересов Не указан. | Conflict of Interest None declared. |
Список литературы / References
- Avtandilov G.G. Ploidometric diagnosis of precancerous processes and the cervical cancer by cytological preparations / G.G. Avtandilov, Yu.K. Glukhova, and I.P. Shabalova // Russian Clinical Laboratory Diagnostics, 2004, no. 11, pp. 45-47.
- Afanasyev M.S. Viral and bacterial nature of dysplasia and the cervical cancer / M.S. Afanasyev, V.A. Aleshkin, S. Afanasyev, et al. // Annals of the Russian Academy of Medical Sciences, 2004, no. 6, pp. 35-40.
- Bazhuttova G.A. The possibilities of the cytological method of research during preventive examination of the cervical material / G.A. Bazhuttova and L.I. Tamarazova // Russian Clinical Laboratory Diagnostics, 2004, no.10, pp. 38-40.
- Belotserkovtseva L.D. A comparative analysis of different methods of treatment of cervical intraepithelial neoplasia associated with HPV infection / L.D. Belotserkovtseva, E.A. Orudzhova, M.N. Shakhlamova et al. // Obstetrics and Gynecology, 2015, vol. 14, no. 5, pp. 55-60.
- A Comprehensive Fight against the Cervical Cancer: Clinical Practice Guide. Geneva: WHO, 2014.
- Dyatlova A.S. Molecular markers of caspase-dependent and mitochondrial apoptosis: a role in the development of pathology and in the processes of cell aging / A.S. Dyatlova, A.V. Dudkov, N.S. Linkova et al. // Advances in Modern Biology, 2018, vol. 138, no. 2, pp. 126-137.
- Kadagidze Z.G. Immunity and Cancer / Z.G. Kadagidze and A.I. Chertkova // Practical Oncology, 2016, vol.17, no. 2, pp. 62-73.
- Bakele M. Localization and functionality of the inflammasome in neutrophils / M. Bakele, M. Joos, S. Burdi et al. // The Journal of Biological Chemistry, vol. 289, no. 8, pp. 5320-5329.
- Creagh E.M. Caspase crosstalk: integration of apoptotic and innate immune signalling pathways / E.M. Creagh // Tren Immunol, 2014, vol. 35, no. 12, pp. 631-639.
- Ciavattini A. Follow up in women with biopsy diagnosis of cervical low-grade squamous intraepithelial lesion (LSIL): how long should it be?,/ A. Ciavattini, N. Clemente, D. Tsiroglou et al. // Arch. Gynecol. Obstet., 2017, vol. 295, nо. 4, pp. 997-1003.
- Jorgensen I. Pyroptotic cell death defends against intracellular pathogens / I. Jorgensen and E.A. Miao // Immunological Reviews, vol. 265, no. 1, pp. 130-142. DOI:10.1111/imr.12287. PMC 4400865. PMID 25879289.
- Kumaresan V. Multifunctional murrel caspase 1, 2, 3, 8 and 9: Conservation, uniqueness and their pathogen-induced expression pattern / V. Kumaresan, G. Ravichandran, F. Nizam et al. // Fish & Shellfish Immunology, 2016, no. 49, pp. 493-504.
- Massad L.S. Updated consensus guidelines for the management of abnormal cervical cancer screening tests and cancer precursors / L.S. Massad, M.H. Einstein, W.K. Huh // ASCCP Consensus Guidelines Conference, J Low Genit Tract Dis, 2013, vol. 17 no. 5, Suppl. 1, pp. 1-27.
- Peng Y.T. Multifaceted role of prohibitin in cell survival and apoptosis / Y.T. Peng, P. Chen, R.Y. Ouyang et al. // Apoptosis, 2015, no. 20(9), pp. 1135-1149.
- Pustavoitau A. Role of senescence marker p16 INK4a measured in peripheral blood T-lymphocytes in predicting length of hospital stay after coronary artery bypass surgery in older adults / A. Pustavoitau, V. Barodka, N.E. Sharpless et al. // Exp Gerontol, 2016, no. 74, pp. 29-36.
- Taniguchi M. Discovery of NKT cells and development of NKT cell-targeted anti-tumor immunotherapy / M. Taniguchi, M. Harada, N. Dashtsoodol et al. // Proc Jpn Acad Ser B Phys Biol Sci, 2015, vol. 91, no. 7, pp. 292-304.
- Teng M.W. From mice to humans: developments in cancer immunoediting / M.W. Teng, J. Galon, W.H. Fridman et al. // J Clin Invest, 2015, vol. 125, no. 9, pp. 3338-3346.
- Tranberg M. Study protocol of the CHOiCE trial: a three-armed, randomized, controlled trial of home-based HPV self-sampling for non-participants in an organized cervical cancer screening program / M. Tranberg, B.H. Bech, J. Blaakær et al. // BMC Cancer, 2016, vol. 16, no. 1, p. 835.
- Zehbe I. Community-randomised controlled trial embedded in the Anishinaabek Cervical Cancer Screening Study: human papillomavirus selfsampling versus Papanicolaou cytology / I. Zehbe, R. Jackson, B. Wood et al. // BMJ Open, 2016, vol. 6, no. 10, pp. 117-154.
- Wong E.L.Y. Evaluation of the impact of human papillomavirus DNA selfsampling on the Uptake of Cervical Cancer Screening / E.L.Y. Wong, K.S. Chan Paul, J.S.Y. Chor et al. // Cancer Nurs, 2016, vol. 39, no. 1, pp. 1-11.
- Vince J.E. The intersection of cell death and inflammasome activation / J.E. Vince and J. Silke // Cellular and Molecular Life Sciences: CMLS, vol.73, no. 11-12), pp. 2349-2367. DOI: 10.1007/s00018-016-2205-2. PMID 27066895.