SILVER-MODIFIED MONTMORILLONITE IN THE TREATMENT OF PATIENTS WITH AN INFECTED WOUND
SILVER-MODIFIED MONTMORILLONITE IN THE TREATMENT OF PATIENTS WITH AN INFECTED WOUND
Abstract
Infection of the skin and soft tissues occupies one of the dominant places among surgical pathology. It is known that about 40% of the total number of patients in surgical hospitals suffer from purulent diseases of the skin and soft tissues. According to statistics, from 500 to 700 thousand people annually in the Russian Federation receive treatment for purulent-inflammatory processes of the skin and soft tissues. The aim of the study was to evaluate the effectiveness of the use of silver–modified montmorillonite in the treatment of skin and soft tissue infections.
Material and Methods. In accordance with the tasks assigned, the following groups of patients were identified: The main group (60 people) used the original silver–modified montmorillonite (Ag-MMT) for local treatment of patients. The control group (52 people) used a silver–containing ATRAUMAN AG dressing for local wound treatment.
Results. In the main group, the complex application of the proposed method of treatment using Ag-MMT made it possible to achieve a pronounced effect in cleansing (4.9 ± 1.1 days) and epithelization (12.2 ± 1.8 days) of the wound compared with the control group (6.2 ± 0.9, 13.8 ± 1.1 days, respectively, p < 0.05). Against the background of treatment, positive dynamics of morphological changes in wounds were revealed in patients of both groups, characterized by a sequential change of cytogram types from necrotic (type I) and degenerative-inflammatory (type II) to inflammatory-regenerative (type IV) in the control group and regenerative (type V) in the main group. The regenerative type of cytograms (type V) was not achieved by the 14th day in the control group, whereas in the main group this type of cytograms was determined by 11.2 ± 1.8 days (p < 0.05).
Conclusions. Studies have shown the clinical effectiveness of the use of silver-modified montmorillonite in the local treatment of purulent wounds. This effect is probably due to a combination of two factors: the absorption property of MMT and the antimicrobial action of silver.
1. Introduction
Currently, wound surgical infection is one of the main problems with which patients seek medical help , , , . The relevance of this problem is also confirmed by the fact that 14.0-16.0% of all nosocomial infections are postoperative wound infections. The vast majority of gram-negative microorganisms, including Pseudomonas aeruginosa, as well as Staphylococcus aureus, according to the results of studies in general surgical hospitals, demonstrate resistance to drugs such as Rivanol, Furacilin, Chloramine and Decamethoxin , , , . At the same time, multicenter studies show that the frequency of wound suppuration after surgical interventions can reach 17.0- 27.0% , , , . Slightly more than 75.0% of hospital rooms are "contaminated" with methicillin-resistant strains of Staphylococcus aureus , , , , 98.0% of chronic wounds are seeded with aerobic organisms , , , . Local treatment of infected wounds includes the use of bioactive dressings, the action of which is mostly strictly directed and carried out in one or another phase of the wound process. On the other hand, since ancient times, silver preparations have been used for the treatment of wound infections, which has a persistent antiseptic effect , , , . Along with the fact that there is more and more data in the literature on the growth of the number of bacteria resistant to modern drugs, the identification of microorganisms resistant to silver preparations is single and scattered , , , . The wounded coatings existing on the market today with immobilized various forms of silver do not provide a stable and sufficient duration of antimicrobial action. At the same time, the results of studies on the high antibacterial activity of nanoscale silver particles began to appear in the literature , , , . Thus, the study of the clinical efficacy of modern materials, including those with the inclusion of silver nanoparticles, in the treatment of skin and soft tissue infection, is an urgent and timely study.
2. Material and methods
In 2020-2021, 112 patients with infectious soft tissue lesions were treated at the surgical infection’s clinic of the Belgorod Regional Clinical Hospital of St. Joasaph. Primary processes were registered in 20 (17.86%), secondary processes – in 92 (82.14%) patients. Of these, 60 are men (53.57%), 52 are women (46.43%).
Upon admission to the department, bacterial agents were found in the wounds of all patients, while the number of colony-forming units ranged from 105 to 109 CFU/ml. In 27.6% of cases, associated wound infection with nosocomial polyresistant strains of bacteria was diagnosed.
The following microorganisms were isolated from the wounds: Staphylococcus aureus – 23.8%; Escherichia coli – 19.23%; Klebsiella pneumoniae – 17.31%; Pseudomonas aeruginosa – 13.46%; Enterococcus faecalis – 9.62%; Staphylococcus epidermidis – 5.77%; Acinetobacter baumannii – 3.85%; Corynebacterium striatum – 3.85%; Staphylococcus haemolyticus– 3.85%.
In accordance with the tasks set, the following groups of patients were identified:
• The main group (60 people) for the local treatment of patients used the original montmorillonite modified with silver (Ag–MMT), obtained at Belgorod State University in laboratory conditions by treating the substance montmorillonite with a solution of silver nitrate (patent No. 2522935. Russian Federation).
• Control group – (52 people) for the local treatment of wounds, a silver-plated ATRAUMAN AG dressing containing silver dressing with antibacterial properties made of polyamide mesh coated with elemental silver was used.
Thus, according to the mechanism of action and composition, these funds are similar and are in states similar in form, which gave us the right to compare their effectiveness with each other.
The distribution of patients in the main and control groups by age and nosological forms is presented in Table 1.
Table 1 - Distribution of patients by age and nosological forms of diseases
Age, years | Group of patients | Total | ||||||||||||||||||||
Main | Control | |||||||||||||||||||||
Primary infections of the skin and soft tissues | Secondary infections of the skin and soft tissues | Primary infections of the skin and soft tissues | Secondary infections of the skin and soft tissues | |||||||||||||||||||
Necrotic cellulite | Necrotic fasciitis | Infected trophic ulcers, Bedsores | Diabetic foot syndrome | Infection of the surgical intervention area | Necrotic cellulite | Necrotic fasciitis | Infected trophic ulcers, Bedsores | Diabetic foot syndrome | Infection of the surgical intervention area | |||||||||||||
абс. | % | абс. | % | абс. | % | абс. | % | абс. | % | абс. | % | абс. | % | абс. | % | абс. | % | абс. | % | абс. | % | |
18-44 | - | - | 1 | 0.89 | - | 9 | 8.04 | - | - | 2 | 1.79 | 4 | 3.57 | 10 | 8.93 | 26 | 23.21 | |||||
45-59 | 3 | 2.68 | - | 1 | 0.89 | - | 7 | 6.25 | 1 | 0.89 | 1 | 0.89 | 2 | 1.79 | 2 | 1.79 | 5 | 4.46 | 22 | 19.64 | ||
60-74 | 5 | 4.46 | 1 | 0.89 | 3 | 2.68 | 1 | 0.89 | 9 | 8.04 | 2 | 1.79 | 1 | 0.89 | 2 | 1.79 | 1 | 0.89 | 7 | 6.25 | 35 | 31.25 |
75-90 | 1 | 0.89 | 1 | 0.89 | 1 | 0.89 | 1 | 0.89 | 6 | 5.36 | 2 | 1.79 | 1 | 0.89 | 4 | 3.57 | 1 | 0.89 | 7 | 6.25 | 25 | 22.32 |
90+ | - | - | 1 | 0.89 | - | 1 | 0.89 | - | 1 | 0.89 | - | - | 1 | 0.89 | 4 | 3.57 | ||||||
Total | 9 | 8.04 | 2 | 1.79 | 7 | 6.25 | 4 | 3.57 | 38 | 33.92 | 4 | 3.57 | 4 | 3.57 | 13 | 12.5 | 8 | 7.14 | 23 | 20.53 | 112 | 100 |

Figure 1 - Infected chest wall wound after treatment with modified silver monmorillonite

Figure 2 - Treatment of an infected foot wound with VAC therapy
Note: Vivano. Hartmann. Germany
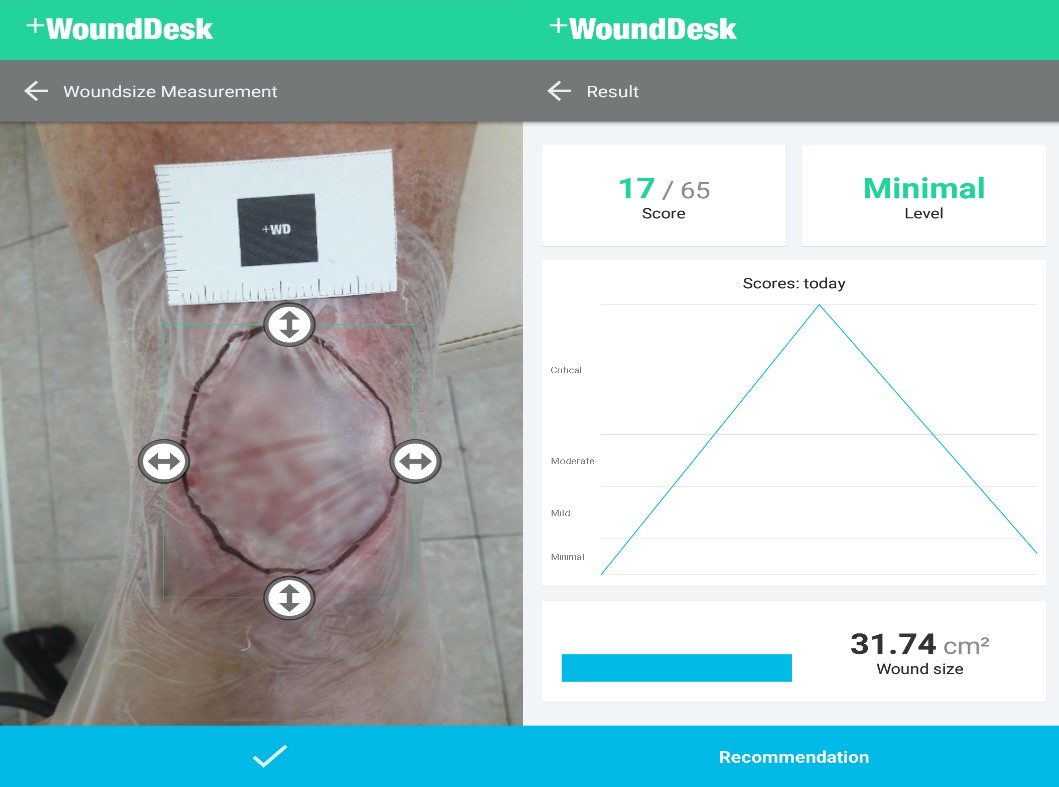
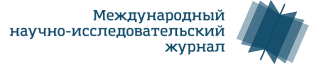
Figure 3 - Determination of the area of the infected ulcer of the lower leg using the mobile app +WoundDesk
Isolation of strains of microorganisms was carried out by standard methods using an automatic bacteriological analyzer VITEK2 (BioMerieux). The sensitivity of microorganisms to antibacterial drugs and the silver form of montmorillonite was determined by the diffusion method. The reading of growth inhibition zones was carried out automatically using the Adagio antibioticogram analyzer. During bacteriological studies, the quantitative composition of the microflora was also determined.
All patients underwent cytological examination of scrapings from the surface of wounds, upon admission, after 7 and 14 days of treatment. The scraping was taken by carefully scraping the surface with a spatula or scalpel. The following types of cytograms were distinguished according to Kamaev M.F.: necrotic, degenerative-inflammatory, inflammatory, inflammatory-regenerative and regenerative.
The work was carried out under the supervision and with the approval of the local ethics committee of the Belgorod Regional Clinical hospital Prelate Ioasaf, Belgorod, Russia (Protocol of February 25, 2020, No. 1); he is the winner of the "YMNIK" program of the Foundation for the Promotion of Innovations in the direction of "Medicine and Health-Saving Technology" in 2021.
Initially, we performed a visual assessment of wounds upon admission to the hospital (initial examination in the dressing room) on the 7th and 14th days of the treatment. The results of the visual assessment of the wounds at the specified study dates are presented in Table 2.
Table 2 - Visual assessment of wounds at all study periods in all 112 patients observed (100%)
Signs | Upon admission | 7th day | 14th day | ||||||||||
Main | Control | Main | Control | Main | Control | ||||||||
абс. | % | абс. | % | абс. | % | абс. | % | абс. | % | абс. | % | ||
Swelling of the paravular area | expressed | 10 | 16.66 | 10 | 19.23 | 3 | 5 | 7 * | 13.46* | 0 | 0 | 3 * | 5.77* |
moderate | 22 | 36.66 | 16 | 30.77 | 13 | 21.67 | 11 | 21.15 | 1 | 1.67 | 7 * | 13.46* | |
pasty | 23 | 38.33 | 20 | 38.46 | 13 | 21.67 | 16 * | 32.69* | 5 | 8.33 | 14 * | 26.92* | |
no | 5 | 8.33 | 6 | 11.54 | 31 | 51.67 | 18 * | 34.62* | 54 | 90 | 28 * | 53.85* | |
Separated from the wound | significant amount | 28 | 46.67 | 26 | 50 | 9 | 15 | 20 | 38.46 | 2 | 3.33 | 6 * | 11.54* |
moderate | 14 | 23.33 | 14 | 26.92 | 5 | 8.33 | 12 * | 23.08* | 2 | 3.33 | 10 * | 19.23* | |
minor | 13 | 21.67 | 7 | 13.46 | 20 | 33.33 | 6 * | 11.54* | 9 | 15 | 14 * | 26.92* | |
no | 5 | 8.33 | 5 | 9.62 | 26 | 43.33 | 14 * | 26.92* | 47 | 78.33 | 22 * | 42.31* | |
Hyperemia of tissues | expressed | 26 | 43.33 | 23 | 44.23 | 8 | 13.33 | 17 * | 32.69* | 0 | 0 | 6 * | 11.54* |
moderate | 28 | 46.67 | 22 | 42.31 | 12 | 20 | 18 * | 34.62* | 1 | 1.67 | 8 * | 15.38* | |
minor | 4 | 6.67 | 5 | 9.62 | 13 | 21.67 | 10 | 19.23 | 8 | 13.33 | 16 * | 30.77* | |
no | 2 | 3.33 | 2 | 3.85 | 27 | 45 | 7 * | 13.46* | 51 | 85 | 22 * | 42.31* | |
Granulation | coarse-grainedthe whole wound) | 0 | 0 | 0 | 0 | 9 | 15 | 2 * | 3.85* | 46 | 76.67 | 28 * | 53.85* |
fine-grainedsingle) | 2 | 3.33 | 2 | 3.85 | 51 | 85 | 40 * | 76.92* | 14 | 23.33 | 16 | 30.77* | |
absent | 58 | 96.67 | 50 | 96.15 | 0 | 0 | 10 * | 19.23* | 0 | 0 | 8 * | 15.38* | |
Marginal epithelization | pronounced distinct border of the epithelium | 0 | 0 | 0 | 0 | 22 | 36.67 | 8 * | 15.38* | 48 | 80 | 19 * | 36.54* |
not expressed | 4 | 6.67 | 4 | 7.69 | 24 | 40 | 16 * | 30.7* | 11 | 18.33 | 24 * | 46.15* | |
absent | 56 | 93.33 | 48 | 92.31 | 14 | 23.33 | 28 * | 53.8* | 1 | 1.67 | 9 * | 17.31* | |
Wound area, cm2 | 62.46 ± 1.2 | 64.21 ± 1.4 | 47.14 ± 1.5 | 58.23 ± 1.9* | 16.30 ± 1.9 | 38.56 ± 1.7* | |||||||
Blood Circulation Temperature IndexTIC) | 5.21 ± 1.2 | 5.94 ± 1.1 | 3.30 ± 0.4 | 4.30 ± 0.5* | 2.20 ± 0.3 | 3.3 ± 0.3* | |||||||
Note: * – the difference is statistically significant, p < 0.05
Upon admission, all patients (both groups) had typical signs for all infected wounds: tissue edema, wound discharge (purulent, purulent-necrotic, etc.), hyperemia of the paravular region (Table 2). There were no significant differences in the frequency of certain signs and their severity in the studied groups.
On the 7th day of the treatment, we noted significant differences in the frequency and nature of such signs as:
- tissue edema (48.3% in the main group, 65.38% in the control group (p < 0.05));
- the number of patients with wound discharge (56.6% in the main group, 73.07% in the control group);
– hyperemia of the paravular region (55% in the main group, 86% in the control group).
Granulations were recorded in all patients of the main group, whereas in the control group granulations appeared in 80.7% of cases (10 patients had no granulation).
Also on the 7th day, we documented the appearance of distinct signs of marginal epithelialization of wounds in 76.6% in the main group and 46.1% in the control group. The area of wounds significantly decreased from (62.46 ± 1.2 cm2) to 47.14 ± 1.5 cm2. in the main group, and in the control group, these indications were 64.21 ± 1.4 cm2 and 58.23 ± 1.9 cm2 (p<0.05), respectively.
On the 14th day of the treatment, further improvement in the characteristics of these signs was recorded in the main group, which was characterized by the absence of tissue edema in 90% of patients, wound discharge in 78.3%, hyperemia of the paravular region in 85% of patients. Pronounced granulation occurred in 100% of patients, epithelialization was detected in 98.3% of patients. The area of the wound decreased by more than 3.8 times in relation to the initial indicators (p < 0.05).
In the control group, similar changes were diagnosed aimed at cleansing and closing wounds, but they were less pronounced, which was characterized by the preservation of tissue edema in 46.1%, wound discharge and tissue hyperemia in 37.6%, granulation was absent in 15.38%, epithelization in 17.31%. The area of the wound was reduced by less than 2 times from the initial figures (p < 0.05).
When analyzing changes in the temperature index of blood circulation, we found a significant decrease of 2.3 times (p < 0.05) by the 14th day of treatment in the main group. In the control group, there was also a decrease in this index to 1.8 times (p < 0.05) from the baseline, these changes were also less pronounced than in the main group (2.2 ± 0.3 in the main and 3.3 ± 0.3 in the control, respectively, p < 0.05).
The analysis of the cytograms of the compared groups against the background of the treatment revealed a significant difference in the composition of cells and types of cytograms compared with the initial data at all study periods (Table 3).
Table 3 - Cytological studies of the dynamics of the reparative process of the wounds
Indicators | Upon admission | 7th day | 14th day | |||
Main | Control | Main | Control | Main | Control | |
Number of white blood cells | 66.7 ± 3.2 | 70.1 ± 2.8 | 38.6 ± 2.8 | 52.3 ± 2.2* | 1.2 ± 0.05 | 16.8 ± 2.6* |
Proportion of destroyed leukocytes,% | 70.2 ± 2.8 | 72 ± 3.2 | 58.2 ± 2.8 | 60.2 ± 2.1 | 0 | 56.2 ± 4.6* |
Cells, % | ||||||
neutrophils | 80.6 ± 3.2 | 78.9 ± 3.2 | 58.5 ± 2.8 | 76.2 ± 1.8* | 2.1 ± 0.08 | 16.3 ± 2.8 |
eosinophils | 0.99 ± 0.05 | 0.88 ± 0.07 | 0.86 ± 0.07 | 0.9 ± 0.07 | 0.86 ± 0.06 | 0.67 ± 0.1 |
lymphocytes | 2.2 ± 0.6 | 2.1 ± 0.7 | 5.6 ± 0.7 | 2.21 ± 0.8* | 16.3 ± 2.1 | 4.1 ± 1.0* |
polyblasts | 7.2 ± 0.3 | 8.6 ± 1.1 | 13.6 ± 1.8 | 10.2 ± 0.9* | 16 ± 1.6 | 11.2 ± 1.2* |
macrophages | 1.2 ± 0.08 | 1.3 ± 1.0 | 8.1 ± 0.72 | 3.9 ± 0.8* | 14.2 ± 2.2 | 6.6 ± 1.6* |
fibroblasts | 0.6 ± 0.08 | 0.8 ± 0.05 | 2.46 ± 0.17 | 1.2 ± 0.2* | 4.6 ± 1.8 | 2.2 ± 0.6* |
multicore cells | 0.03 ± 0.01 | 0.038 ± 0.01 | 0.05 ± 0.01 | 0.04 ± 0.01 | 0.06 ± 0.01 | 0.07*0.02 |
epithelium | 0 | 0 | units | 0 | cell groups | cell groups |
Note: * – the difference is statistically significant, p < 0.05
When there were no significant differences in the cytograms of the compared groups. Changes characteristic of type I cytograms (necrotic type) were noted in all preparations: the visual fields are represented by destroyed neutrophils, a single number of microphages with no esterase activity, erythrocytes, microorganisms, as well as tissue detritus (Figure 4).
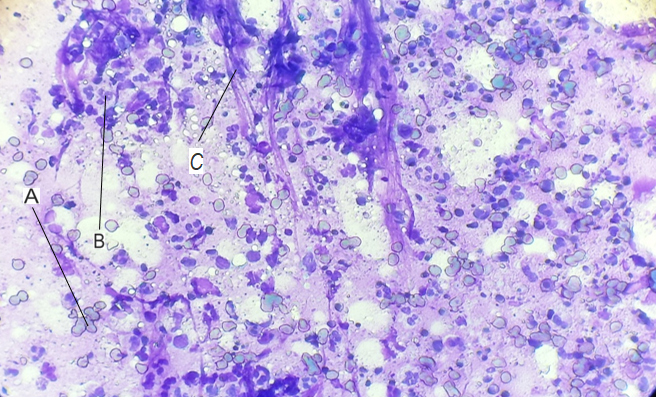
Figure 4 - Upon admission
Note: a – erythrocytes; b – neutrophils; c – fibrin
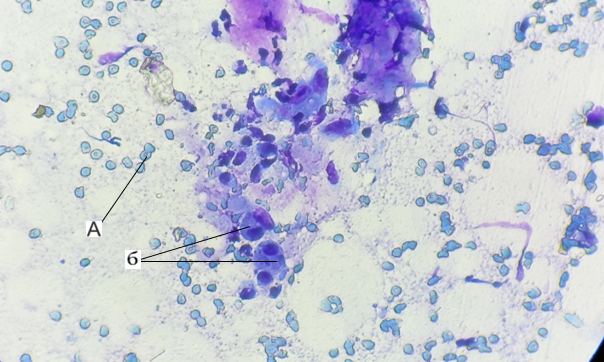
Figure 5 - On 7th day
Note: a – erythrocytes; b – macrophages
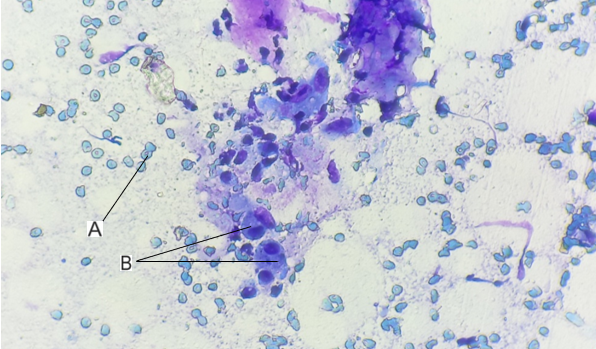
Figure 6 - On 14th day
Note: a – erythrocytes; b – macrophages
3. Discussion
In the main group, the complex application of the proposed method of treatment using Ag-MMT made it possible to achieve a pronounced effect in cleansing (4.9 ± 1.1 days) and epithelization (12.2 ± 1.8 days) of the wound compared with the control group (6.2 ± 0.9, 13.8 ± 1.1 days, respectively, p < 0.05). Against the background of treatment, positive dynamics of morphological changes in wounds were revealed in patients of both groups, characterized by a sequential change from cytograms of types I and II (necrotic, degenerative-inflammatory) to type IV in the control and type V in the main groups (inflammatory-regenerative and regenerative, respectively). The regenerative type of cytograms (type V) was not achieved by the 14th day in the control group, whereas in the main group this type of cytograms was determined by 11.2 ± 1.8 days (p < 0.05).
4. Conclusion
Thus, studies have shown the clinical effectiveness of the use of silver-modified montmorillonite in the local treatment of purulent wounds. This effect is probably due to a combination of two factors: the absorption properties of MMT and the antimicrobial action of silver.